Mild cognitive impairment (MCI) is the stage between the expected cognitive decline of normal aging and the more serious decline of dementia. It's characterized by problems with memory, language, thinking or judgment.
If you have mild cognitive impairment, you may be aware that your memory or mental function has "slipped." Your family and close friends also may notice a change. But these changes aren't severe enough to significantly interfere with your daily life and usual activities.
Mild cognitive impairment may increase your risk of later developing dementia caused by Alzheimer's disease or other neurological conditions. But some people with mild cognitive impairment never get worse, and a few eventually get better.
Symptoms
Your brain, like the rest of your body, changes as you grow older. Many people notice gradually increasing forgetfulness as they age. It may take longer to think of a word or to recall a person's name.
But consistent or increasing concern about your mental performance may suggest mild cognitive impairment (MCI). Cognitive issues may go beyond what's expected and indicate possible MCI if you experience any or all of the following:
- You forget things more often.
- You forget important events such as appointments or social engagements.
- You lose your train of thought or the thread of conversations, books or movies.
- You feel increasingly overwhelmed by making decisions, planning steps to accomplish a task or understanding instructions.
- You start to have trouble finding your way around familiar environments.
- You become more impulsive or show increasingly poor judgment.
- Your family and friends notice any of these changes.
If you have MCI, you may also experience:
- Depression
- Irritability and aggression
- Anxiety
- Apathy
Causes
There's no single cause of mild cognitive impairment (MCI), just as there's no single outcome for the disorder. Symptoms of MCI may remain stable for years, progress to Alzheimer's disease or another type of dementia, or improve over time.
Current evidence indicates that MCI often, but not always, develops from a lesser degree of the same types of brain changes seen in Alzheimer's disease or other forms of dementia. Some of these changes have been identified in autopsy studies of people with MCI. These changes include:
- Abnormal clumps of beta-amyloid protein (plaques) and microscopic protein clumps of tau characteristic of Alzheimer's disease (tangles)
- Lewy bodies, which are microscopic clumps of another protein associated with Parkinson's disease, dementia with Lewy bodies and some cases of Alzheimer's disease
- Small strokes or reduced blood flow through brain blood vessels
Brain-imaging studies show that the following changes may be associated with MCI:
- Shrinkage of the hippocampus, a brain region important for memory
- Enlargement of the brain's fluid-filled spaces (ventricles)
- Reduced use of glucose, the sugar that's the primary source of energy for cells, in key brain regions
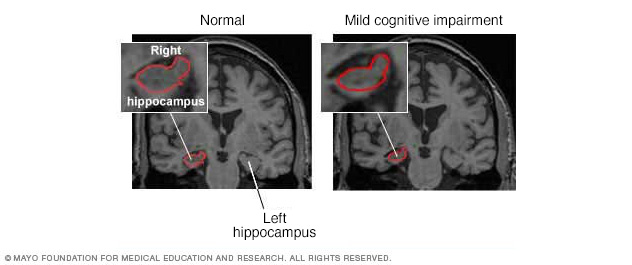
These MRIs reveal shrinkage of the hippocampus, a part of the brain associated with memory, during the transition from normal cognitive function to mild cognitive impairment. The inset on each MRI is an enlarged view of the right hippocampus.
Risk factors
The strongest risk factors for MCI are:
- Increasing age
- Having a specific form of a gene known as APOE e4, also linked to Alzheimer's disease — though having the gene doesn't guarantee that you'll experience cognitive decline
Other medical conditions and lifestyle factors have been linked to an increased risk of cognitive change, including:
- Diabetes
- Smoking
- High blood pressure
- Elevated cholesterol
- Obesity
- Depression
- Lack of physical exercise
- Low education level
- Infrequent participation in mentally or socially stimulating activities
Complications
People with MCI have a significantly increased risk — but not a certainty — of developing dementia. Overall, about 1% to 3% of older adults develop dementia every year. Studies suggest that around 10% to 15% of individuals with MCI go on to develop dementia each year.
Prevention
Mild cognitive impairment can't always be prevented. But research has found some environmental factors that may affect the risk of developing the condition. Studies show that these steps may help prevent cognitive impairment:
- Avoid excessive alcohol use.
- Limit exposure to air pollution.
- Reduce your risk of head injury.
- Don't smoke.
- Manage health conditions such as diabetes, high blood pressure, obesity and depression.
- Practice good sleep hygiene and manage sleep disturbances.
- Eat a nutrient-rich diet that has plenty of fruits and vegetables and is low in saturated fats.
- Engage socially with others.
- Exercise regularly at a moderate to vigorous intensity.
- Wear a hearing aid if you have hearing loss.
- Stimulate your mind with puzzles, games and memory training.
Diagnosis
There is no specific test to confirm a diagnosis of mild cognitive impairment (MCI). Your doctor will decide whether MCI is the most likely cause of your symptoms based on the information you provide and results of various tests that can help clarify the diagnosis.
Many doctors diagnose MCI based on the following criteria developed by a panel of international experts:
- You have problems with memory or another mental function. You may have problems with your memory, planning, following instructions or making decisions. Your own impressions should be confirmed by someone close to you.
- You've declined over time. A careful medical history reveals that your mental function has declined from a higher level. This change ideally is confirmed by a family member or a close friend.
- Your overall mental function and daily activities aren't affected. Your medical history shows that overall your daily activities generally aren't impaired, although specific symptoms may cause worry and inconvenience.
- Mental status testing shows a mild level of impairment for your age and education level. Doctors often assess mental performance with a brief test such as the Short Test of Mental Status, the Montreal Cognitive Assessment (MoCA) or the Mini-Mental State Examination (MMSE). More-detailed neuropsychological testing may help determine the degree of memory impairment, which types of memory are most affected and whether other mental skills also are impaired.
- Your diagnosis isn't dementia. The problems that you describe and that your doctor documents through corroborating reports, your medical history, and mental status testing aren't severe enough to be diagnosed as Alzheimer's disease or another type of dementia.
Neurological exam
As part of your physical exam, your doctor may perform some basic tests that indicate how well your brain and nervous system are working. These tests can help detect neurological signs of Parkinson's disease, strokes, tumors or other medical conditions that can impair your memory as well as your physical function. The neurological exam may test:
- Reflexes
- Eye movements
- Walking and balance
Lab tests
Blood tests can help rule out physical problems that can affect memory, such as a vitamin B-12 deficiency or an underactive thyroid gland.
Brain imaging
Your doctor may order an MRI or CT scan to check for evidence of a brain tumor, stroke or bleeding.
Mental status testing
Short forms of mental status testing can be done in about 10 minutes. During testing, doctors ask people to conduct several specific tasks and answer several questions, such as naming today's date or following a written instruction.
Longer forms of neuropsychological testing can provide additional details about your mental function compared with the function of others of a similar age and education level. These tests may also help identify patterns of change that offer clues about the underlying cause of your symptoms.
Treatment
Currently, no drugs or other treatments are approved specifically for mild cognitive impairment (MCI) by the Food and Drug Administration (FDA). However, MCI is an active area of research. Clinical studies are underway to better understand the disorder and find treatments that may improve symptoms or prevent or delay progression to dementia.
Alzheimer's drugs
Doctors sometimes prescribe cholinesterase inhibitors, a type of drug approved for Alzheimer's disease, for people with MCI whose main symptom is memory loss. However, cholinesterase inhibitors aren't recommended for routine treatment of MCI. They haven't been found to affect progression to dementia, and can cause side effects.
Treating reversible causes of MCI: Medications
Certain medications can cause side effects that affect cognitive function. These side effects are thought to go away once the medication is stopped. It's important to discuss any side effects with your doctor and never stop taking your medications unless your doctor instructs you to do so. These medications include:
- Benzodiazepines, used to treat conditions such as anxiety, seizures and sleep disturbances
- Anticholinergics, which affect chemicals in the nervous system to treat many different types of conditions
- Antihistamines, often used to manage allergy symptoms
- Opioids, often used to treat pain
- Proton pump inhibitors, often used to treat reflux or gastroesophageal reflux disease (GERD)
Treating reversible causes of MCI: Other conditions
Other common conditions besides MCI can make you feel forgetful or less mentally sharp than usual. Treating these conditions can help improve your memory and overall mental function. Conditions that can affect memory include:
- High blood pressure. People with MCI tend to be more likely to have problems with the blood vessels inside their brains. High blood pressure can worsen these problems and cause memory difficulties. Your doctor will monitor your blood pressure and recommend steps to lower it if it's too high.
- Depression. When you're depressed, you often feel forgetful and mentally "foggy." Depression is common in people with MCI. Treating depression may help improve memory, while making it easier to cope with the changes in your life.
- Sleep apnea. In this condition, your breathing repeatedly stops and starts while you're asleep, making it difficult to get a good night's rest. Sleep apnea can make you feel excessively tired during the day, forgetful and unable to concentrate. Treatment can improve these symptoms and restore alertness.
Lifestyle and home remedies
Study results have been mixed about whether diet, exercise or other healthy lifestyle choices can prevent or reverse cognitive decline. Regardless, these healthy choices promote good overall health and may play a role in good cognitive health.
- Regular physical exercise has known benefits for heart health and may also help prevent or slow cognitive decline.
- A diet low in fat and rich in fruits and vegetables is another heart-healthy choice that also may help protect cognitive health.
- Omega-3 fatty acids also are good for the heart. Most research showing a possible benefit for cognitive health uses fish consumption as a yardstick for the amount of omega-3 fatty acids eaten.
- Intellectual stimulation may prevent cognitive decline. Studies have shown that computer use, playing games, reading books and other intellectual activities may help preserve function and prevent cognitive decline.
- Social engagement may make life more satisfying, help preserve mental function and slow mental decline.
- Memory training and other cognitive training may help improve your function.
Alternative medicine
Some supplements — including vitamin E, ginkgo and others — have been suggested to help prevent or delay the progression of mild cognitive impairment. However, no supplement has shown any benefit in a clinical trial.
Preparing for an appointment
You're likely to start by seeing your family doctor. If your doctor suspects that you have cognitive changes, you may be referred to a specialist with expertise in evaluating mental function. This specialist may be a neurologist, psychiatrist or neuropsychologist.
Because appointments can be brief and there's often a lot to talk about, it's good to be well prepared. Here are some suggestions to help you get ready for your appointment and know what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. When you make your appointment, ask if you need to fast for bloodwork or if you need to do anything else to prepare for diagnostic tests.
- Write down all of your symptoms. Your doctor will want to know details about what's causing your concern about your memory or mental function. Make notes about some of the most important examples of forgetfulness or other lapses you want to mention. Try to remember when you first started to suspect that something might be wrong. If you think your difficulties are getting worse, be ready to explain why.
- Take along a family member or friend, if possible. Corroboration from a relative or trusted friend can play a key role in confirming that your memory difficulties are apparent to others. Having someone along can also help you remember all the information provided during your appointment.
- Make a list of your other medical conditions. Your doctor will want to know if you're currently being treated for diabetes, heart disease, past strokes or any other conditions.
- Make a list of all your medications. Your doctor will want to know about any prescription and over-the-counter drugs, vitamins or supplements you're taking.
Questions to ask your doctor
Because time with your doctor is limited, writing down a list of questions will help you make the most of your appointment. List your questions from most pressing to least important in case time runs out. For cognitive changes, some questions to ask your doctor include:
- Do I have a memory problem?
- What's causing my difficulties?
- What tests do I need?
- Do I need to see a specialist? What will that cost? Will my insurance cover it?
- Are treatments available?
- Are there any clinical trials of experimental treatments I should consider?
- Should I expect any long-term complications?
- Will my new symptoms affect how I manage my other health conditions?
- Do I need to follow any restrictions?
- Is there a generic alternative to the medicine you're giving me?
- Do you have any brochures or other printed material I can take home with me? What websites do you recommend?
In addition to the questions you've prepared ahead of time, don't hesitate to ask your doctor to clarify anything you don't understand.
What to expect from your doctor
Your doctor is also likely to have questions for you. Being ready to respond may free up time to focus on any points you want to talk about in-depth. Your doctor may ask:
- What kinds of memory difficulties are you having? When did they first appear?
- Are they steadily getting worse, or are they sometimes better and sometimes worse?
- Do you feel any sadder or more anxious than usual?
- Have you noticed any changes in the way you react to people or events?
- Have you noticed any changes in how well or how long you sleep? Do you snore?
- Do you have more energy than usual, less than usual or about the same?
- What medications are you taking? Are you taking any vitamins or supplements?
- Do you drink alcohol? How much?
- What other medical conditions are you being treated for?
- Have you noticed any trembling or trouble walking?
- Are you having any trouble remembering your medical appointments or when to take your medication?
- Have you had your hearing and vision tested recently?
- Did anyone else in your family ever have memory trouble? Was anyone ever diagnosed with Alzheimer's disease or dementia?
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.