Pulmonary hypertension is a type of high blood pressure that affects the arteries in the lungs and the right side of the heart.
In one form of pulmonary hypertension, called pulmonary arterial hypertension (PAH), blood vessels in the lungs are narrowed, blocked or destroyed. The damage slows blood flow through the lungs, and blood pressure in the lung arteries rises. The heart must work harder to pump blood through the lungs. The extra effort eventually causes the heart muscle to become weak and fail.
In some people, pulmonary hypertension slowly gets worse and can be life-threatening. Although there's no cure for some types of pulmonary hypertension, treatment can help reduce symptoms and improve quality of life.
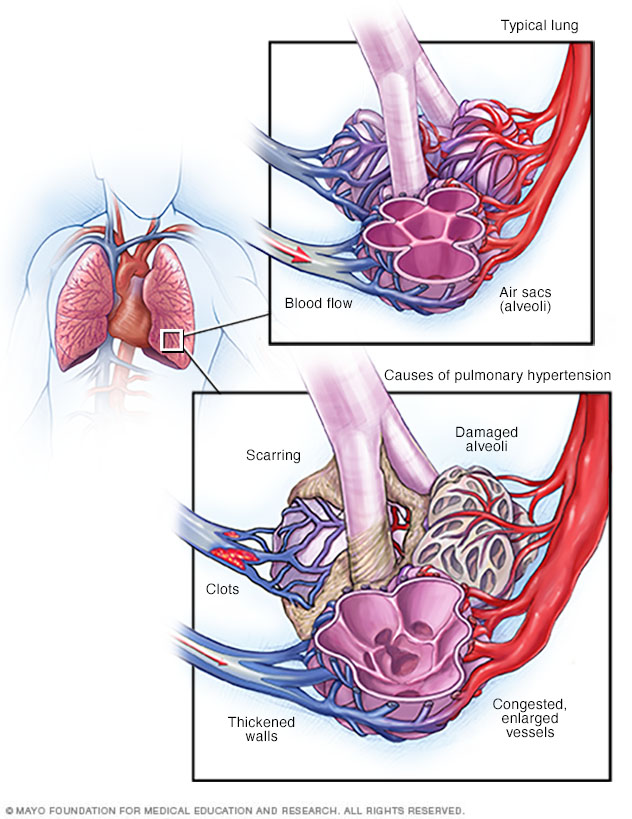
When blood vessels in the lungs become thickened, narrowed, blocked or destroyed, it's harder for blood to flow through the lungs. As a result, blood pressure increases in the lungs, a condition called pulmonary hypertension.
Symptoms
The signs and symptoms of pulmonary hypertension develop slowly. You may not notice them for months or even years. Symptoms get worse as the disease progresses.
Pulmonary hypertension signs and symptoms include:
- Blue lips and skin (cyanosis)
- Chest pressure or pain
- Dizziness or fainting spells (syncope)
- Fast pulse or pounding heartbeat (palpitations)
- Fatigue
- Shortness of breath (dyspnea), initially while exercising and eventually while at rest
- Swelling (edema) in the ankles, legs and eventually the belly area (abdomen)
Causes
The typical heart has two upper chambers (atria) and two lower chambers (ventricles). Each time blood passes through the heart, the lower right chamber (right ventricle) pumps blood to the lungs through a large blood vessel (pulmonary artery).
In the lungs, the blood releases carbon dioxide and picks up oxygen. The blood typically flows easily through blood vessels in the lungs (pulmonary arteries, capillaries and veins) to the left side of the heart.
However, changes in the cells that line the pulmonary arteries can cause the walls of the arteries to become stiff, swollen and thick. These changes may slow down or block blood flow through the lungs, causing pulmonary hypertension.
Pulmonary hypertension is classified into five groups, depending on the cause.
Group 1: Pulmonary arterial hypertension (PAH)
Causes include:
- Unknown cause (idiopathic pulmonary arterial hypertension)
- Changes in a gene passed down through families (heritable pulmonary arterial hypertension)
- Use of certain drugs or illegal substances
- Heart problems present at birth (congenital heart disease)
- Other conditions such as HIV infection, chronic liver disease (cirrhosis) and connective tissue disorders (scleroderma, lupus, others)
Group 2: Pulmonary hypertension caused by left-sided heart disease
Causes include:
- Left-sided heart valve disease such as mitral valve or aortic valve disease
- Failure of the lower left heart chamber (left ventricle)
Group 3: Pulmonary hypertension caused by lung disease
Causes include:
- Chronic obstructive pulmonary disease (COPD)
- Scarring of the tissue between the lung's air sacs (pulmonary fibrosis)
- Obstructive sleep apnea
- Long-term exposure to high altitudes in people who may be at higher risk of pulmonary hypertension
Group 4: Pulmonary hypertension caused by chronic blood clots
Causes include:
- Chronic blood clots in the lungs (pulmonary emboli)
- Other clotting disorders
Group 5: Pulmonary hypertension triggered by other health conditions
Causes include:
- Blood disorders, including polycythemia vera and essential thrombocythemia
- Inflammatory disorders such as sarcoidosis and vasculitis
- Metabolic disorders, including glycogen storage disease
- Kidney disease
- Tumors pressing against pulmonary arteries
Eisenmenger syndrome and pulmonary hypertension
Eisenmenger syndrome is a type of congenital heart disease that causes pulmonary hypertension. It's most commonly caused by a large hole in the heart between the two lower heart chambers (ventricles), called a ventricular septal defect.
This hole in the heart causes blood to flow incorrectly in the heart. Oxygen-carrying blood (red blood) mixes with oxygen-poor blood (blue blood). The blood then returns to the lungs — instead of going to the rest of the body — increasing the pressure in the pulmonary arteries and causing pulmonary hypertension.

A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
Risk factors
Pulmonary hypertension is more often diagnosed in people ages 30 to 60. Growing older can increase the risk of developing Group 1 pulmonary hypertension, called pulmonary arterial hypertension (PAH). However, PAH from an unknown cause (idiopathic PAH) is more common in younger adults.
Other things that can raise the risk of pulmonary hypertension include:
- A family history of the condition
- Being overweight
- Blood-clotting disorders or a family history of blood clots in the lungs
- Exposure to asbestos
- Congenital heart disease
- Living at a high altitude
- Use of certain drugs, including some weight-loss medicines and illegal drugs such as cocaine or methamphetamine
- Use of selective serotonin reuptake inhibitors (SSRIs), used to treat depression and anxiety
Complications
Potential complications of pulmonary hypertension include:
-
Right-sided heart enlargement and heart failure (cor pulmonale). In cor pulmonale, the heart's right lower chamber (ventricle) becomes enlarged. It has to pump harder than usual to move blood through narrowed or blocked pulmonary arteries.
As a result, the heart walls thicken and the right ventricle expands to increase the amount of blood it can hold. But these changes create more strain on the heart, and eventually the right ventricle fails.
- Blood clots. Having pulmonary hypertension increases the risk of blood clots in the small arteries in the lungs.
- Irregular heartbeats (arrhythmias). Certain arrhythmias caused by pulmonary hypertension can be life-threatening.
- Bleeding in the lungs. Pulmonary hypertension can lead to life-threatening bleeding into the lungs and coughing up blood (hemoptysis).
- Pregnancy complications. Pulmonary hypertension can be life-threatening for a developing baby.
Diagnosis
Pulmonary hypertension is hard to diagnose early because it's not often detected during a routine physical exam. Even when pulmonary hypertension is more advanced, its signs and symptoms are similar to those of other heart and lung conditions.
To diagnose pulmonary hypertension, a health care provider will perform a physical exam and review your symptoms. You'll likely be asked questions about your medical and family history.
Blood and imaging tests done to help diagnose pulmonary hypertension may include:
- Blood tests. Blood tests can help determine the cause of pulmonary hypertension or detect signs of complications.
- Chest X-ray. A chest X-ray creates pictures of the heart, lungs and chest. A chest X-ray may be used to check for other lung conditions that can cause pulmonary hypertension.
- Electrocardiogram (ECG). This simple test records the electrical activity of the heart. It can detect changes in the heartbeat. Patterns on an ECG may reveal signs of right ventricle enlargement or strain.
-
Echocardiogram. Sound waves are used to create moving images of the beating heart. An echocardiogram shows blood flow through the heart. This test may be done to help diagnose pulmonary hypertension or to determine how well treatments are working.
Sometimes, an echocardiogram is done while exercising on a stationary bike or treadmill to learn how activity affects the heart. If you have this test, you may be asked to wear a mask that checks how well the heart and lungs use oxygen and carbon dioxide.
-
Right heart catheterization. If an echocardiogram reveals pulmonary hypertension, you'll likely have a right heart catheterization to confirm the diagnosis.
During this procedure, a cardiologist places a thin, flexible tube (catheter) into a blood vessel, usually in the groin. The catheter is gently guided into the right lower heart chamber (right ventricle) and pulmonary artery. A cardiologist can then measure blood pressure in the main pulmonary arteries and the right ventricle.
Other tests may be done to check the condition of the lungs and pulmonary arteries and further determine the cause of pulmonary hypertension:
-
Computerized tomography (CT). This imaging test takes a series of X-rays to create cross-sectional pictures of the bones, blood vessels and soft tissues inside the body. Dye (contrast) may be injected into a vein to help the blood vessels show up more clearly on the images.
A heart (cardiac) CT scan can show the size of the heart and any blockages in the pulmonary arteries. It can help diagnose lung diseases that might lead to pulmonary hypertension such as COPD or pulmonary fibrosis.
- Magnetic resonance imaging (MRI). This test uses magnetic fields and radio waves to create detailed images of the heart. It can show blood flow in the pulmonary arteries and determine how well the lower right heart chamber (right ventricle) is working.
- Lung (pulmonary) function test. This noninvasive test measures how much air the lungs can hold and the airflow in and out of the lungs. The test involves blowing into an instrument called a spirometer.
- Sleep study (polysomnogram). A sleep study measures brain activity, heart rate, blood pressure, oxygen levels and other factors during sleep. A sleep study can help diagnose obstructive sleep apnea, which can cause pulmonary hypertension.
- Ventilation/perfusion (V/Q) scan. In this test, a radioactive tracer is given by IV. The tracer shows blood flow and airflow to the lungs. A V/Q scan can determine whether blood clots are causing symptoms of pulmonary hypertension.
- Open-lung biopsy. Rarely, an open-lung biopsy may be done to check for a possible cause of pulmonary hypertension. An open-lung biopsy is a type of surgery in which a small sample of tissue is removed from the lungs.
Genetic testing
If a family member has had pulmonary hypertension, screening for genes that are linked with disease may be recommended. If you test positive, your health care provider might recommend screening other family members.
Pulmonary hypertension functional classification
Once a diagnosis of pulmonary hypertension is confirmed, the condition is classified according to how the symptoms affect you and your ability to do everyday tasks.
Functional classifications of pulmonary hypertension fall into one of following categories:
- Class I. Pulmonary hypertension is diagnosed, but there are no symptoms during rest or exercise.
- Class II. There are no symptoms at rest. Everyday chores or activities such as going to work or the grocery store may cause some shortness of breath or mild chest pain. There's a slight limitation of physical activity.
- Class III. It's comfortable at rest, but doing simple tasks such as bathing, dressing or preparing meals causes fatigue, shortness of breath and chest pain. The ability to do physical activity becomes very limited.
- Class IV. Symptoms occur at rest and during physical activity. Any type of activity causes increasing discomfort.
Treatment
There's no cure for pulmonary hypertension, but treatment is available to help improve signs and symptoms and slow the progress of the disease.
It often takes some time to find the most appropriate treatment for pulmonary hypertension. The treatments are often complex and require extensive follow-up care.
When pulmonary hypertension is caused by another condition, treatment is given for the underlying cause whenever possible.
Medications
Medications are available to help improve symptoms of pulmonary hypertension and to slow the progression of the disease.
Medications that may be prescribed to treat pulmonary hypertension symptoms or complications include:
-
Blood vessel dilators (vasodilators). This type of medicine relaxes and opens narrowed blood vessels, improving blood flow. Vasodilators may be taken by mouth, inhaled, injected or given by IV infusion. A commonly prescribed vasodilator for pulmonary hypertension is epoprostenol (Flolan, Veletri).
This drug continuously flows through an IV attached to a small pump, which is worn in a pack on the belt or shoulder. Potential side effects of epoprostenol include jaw pain, nausea, diarrhea, leg cramps, and pain and infection at the IV site.
Other types of vasodilators, including treprostinil (Tyvaso, Remodulin, Orenitram), can be inhaled, injected or taken by mouth. The drug iloprost (Ventavis) is given while breathing in through a nebulizer, a machine that vaporizes the medication.
Side effects associated with treprostinil include chest pain, often with headache and nausea, and breathlessness. Possible side effects of iloprost include headache, nausea and diarrhea.
- Guanylate cyclase (GSC) stimulators. This type of medicine increases nitric oxide in the body, which relaxes the pulmonary arteries and lowers pressure in the lungs. GSC stimulators include riociguat (Adempas). Side effects include nausea, dizziness and fainting. You should not take GSC stimulators if you're pregnant.
- Medications to widen blood vessels. Medications called endothelin receptor antagonists reverse the effect of a substance in the walls of blood vessels that causes them to narrow. Such drugs include bosentan (Tracleer), macitentan (Opsumit) and ambrisentan (Letairis). They may improve energy level and symptoms. However, they can damage the liver. Monthly blood tests may be done to check liver function. Don't take these drugs during pregnancy.
- Medications to increase blood flow. Drugs called phosphodiesterase 5 (PDE5) inhibitors may be used to increase blood flow through the lungs. These medicines are also used to treat erectile dysfunction. They include sildenafil (Revatio, Viagra) and tadalafil (Adcirca, Cialis, Alyq).
- High-dose calcium channel blockers. These drugs help relax the muscles in the walls of blood vessels. They include amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and nifedipine (Procardia). Although calcium channel blockers can be effective, only a small number of people with pulmonary hypertension improve while taking them.
-
Blood thinners (anticoagulants). Warfarin (Jantoven) may be prescribed to help prevent blood clots. Blood thinners increase the risk of bleeding, especially in those who are having surgery or an invasive procedure. If you take blood thinners, you'll need occasional blood tests to see if the medicine is working as it should. Don't stop taking blood thinners without first talking to your care provider.
Many other drugs, herbal supplements and foods can interact with warfarin. Always tell your provider about your diet and all the medications you take, including those bought without a prescription.
- Digoxin (Lanoxin). This medicine helps the heart beat stronger and pump more blood. It can help control irregular heartbeats (arrhythmias).
- Water pills (diuretics). These medications help the kidneys remove excess fluid from the body. This reduces the amount of work the heart has to do. Diuretics may also be used to reduce fluid buildup in the lungs, legs and abdomen.
- Oxygen therapy. Breathing pure oxygen is sometimes recommended as a treatment for pulmonary hypertension, especially for those who live at a high altitude or have sleep apnea. Continuous oxygen therapy may be needed.
Surgery and other procedures
If medications do not help control the signs and symptoms of pulmonary hypertension, surgery may be recommended. Surgeries to treat pulmonary hypertension include:
- Atrial septostomy. This open-heart surgery may be recommended if medications don't control pulmonary hypertension signs and symptoms. In an atrial septostomy, a surgeon creates an opening between the upper left and right chambers of the heart (atria) to relieve the pressure on the right side of the heart. Potential complications include heart rhythm problems (arrhythmias).
-
Lung or heart-lung transplant. Sometimes, a lung or heart-lung transplant may be recommended, especially for younger people who have idiopathic pulmonary arterial hypertension.
Major risks of any type of transplantation include rejection of the transplanted organ and serious infection. Immunosuppressant drugs must be taken for life to help reduce the chance of rejection.
Lifestyle and home remedies
Although medical treatment can't cure pulmonary hypertension, it can lessen symptoms. Lifestyle changes also may help improve pulmonary hypertension. Consider these tips:
- Get plenty of rest. Resting can reduce fatigue related to pulmonary hypertension.
- Stay as active as possible. Even the mildest forms of activity might be too exhausting for some people who have pulmonary hypertension. For others, moderate exercise, such as walking, might be beneficial — especially when done during oxygen therapy. Usually, it's recommended that people with pulmonary hypertension not lift heavy weights. Your provider can help you plan an appropriate exercise program.
- Don't smoke. If you smoke, the most important thing you can do for your heart and lungs is to stop. If you can't stop smoking by yourself, ask your health care provider to prescribe a treatment plan to help you quit. Also, avoid secondhand smoke if possible.
- Talk to a health care provider before becoming pregnant. Pulmonary hypertension can cause serious complications to both mom and her baby during pregnancy. Birth control pills can increase the risk of blood clots. Talk to your health care provider about alternative forms of birth control.
- Avoid high altitudes. High altitudes can make pulmonary hypertension worse. If you live at an altitude of 8,000 feet (2,438 meters) or higher, your care provider might recommend that you move to a lower altitude.
- Avoid situations that can excessively lower blood pressure. These include sitting in a hot tub or sauna or taking long hot baths or showers. Such activities lower blood pressure and can cause fainting or even death. Also avoid activities that cause prolonged straining, such as lifting heavy objects or weights.
- Eat healthy and manage weight. Eat a healthy diet rich in whole grains, fruits and vegetables, lean meats, and low-fat dairy products. Avoid saturated fat, trans fat and cholesterol. Limit salt. Aim to maintain a healthy weight.
- Review all medications with your health care provider. Tell your provider about all the medications you take, including those bought without a prescription. Some medications can make pulmonary hypertension worse or interfere with its treatment. Take all your medications as prescribed. Your care provider may work with another specialist to determine and manage the best drug treatment for pulmonary hypertension.
- Get regular health checkups. Tell your provider about any new or worsening symptoms or medication side effects. If pulmonary hypertension affects your quality of life, ask about options that could help.
- Get recommended vaccines. Respiratory infections can cause serious health concerns for people with pulmonary hypertension. Ask your provider about recommend vaccines to prevent common viral infections.
- Get support. Connecting with others who are going through similar situations may help you ease and manage stress. Ask your provider if there are any pulmonary hypertension support groups in your area.
Preparing for an appointment
If you think that you might have pulmonary hypertension or are worried about your pulmonary hypertension risk, make an appointment with your health care provider.
While shortness of breath is one of the first symptoms of pulmonary hypertension, the symptom is also common with many other conditions, such as asthma.
Appointments can be brief. There's often a lot to discuss, so it's a good idea to be prepared for your appointment. Here's some information to help you get ready for your appointment, and what to expect from your provider.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as fill out forms or restrict your diet. For some imaging tests, for example, you might need to avoid food or drink for a period of time beforehand.
- Write down any symptoms you're having, including any that might seem unrelated to pulmonary hypertension. Try to remember when they began. Be specific, such as days, weeks and months.
- Write down key personal information, including any family history of pulmonary hypertension, lung disease, heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes.
- Make a list of all medications, as well as any vitamins or supplements that you're taking. Also, be sure to tell your provider if you've recently stopped taking any medications.
- Take a family member or friend along, if possible. Sometimes it can be difficult to remember all the information provided to you during an appointment. Someone who comes with you might remember something that you missed or forgot.
- Be prepared to discuss your diet and exercise habits. If you don't already follow a diet or exercise routine, talk to your provider about any challenges you might face in getting started.
- Write down questions to ask your health care provider. List your questions from most important to least important in case time runs out.
For pulmonary hypertension, some basic questions to ask your health care provider include:
- What is likely causing my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What kinds of tests will I need?
- What's the most appropriate treatment?
- What's an appropriate level of physical activity?
- How often should I be screened for changes in my condition?
- What are the alternatives to the primary approach that you're suggesting?
- I have other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your health care provider is likely to ask you many questions. Being ready to answer them might save time to go over any details you want to spend more time on. Your provider might ask:
- When did you first begin having symptoms?
- Do you always have symptoms or do they come and go?
- How severe are the symptoms?
- What, if anything, seems to improve symptoms?
- What, if anything, seems to worsen symptoms?
What you can do in the meantime
It's never too late to make healthy lifestyle changes, such as quitting smoking, cutting down on salt and eating a healthy diet. These changes may help prevent pulmonary hypertension from getting worse.
Copyright © 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.