Spontaneous coronary artery dissection — sometimes referred to as SCAD — is an emergency condition that occurs when a tear forms in a blood vessel in the heart.
SCAD can slow or block blood flow to the heart, causing a heart attack, heart rhythm problems (arrythmias) or sudden death.
SCAD most commonly affects women in their 40s and 50s, though it can occur at any age and can occur in men. People who have SCAD often don't have risk factors for heart disease, such as high blood pressure, high cholesterol or diabetes.
SCAD can cause sudden death if it isn't diagnosed and treated promptly. Seek emergency attention if you have heart attack symptoms — even if you think you aren't at risk of a heart attack.
Symptoms
Symptoms of SCAD can include:
- Chest pain
- A rapid heartbeat or fluttery feeling in the chest
- Pain in the arms, shoulders, back or jaw
- Shortness of breath
- Sweating
- Unusual, extreme tiredness
- Nausea
- Dizziness
When to see a doctor
If you have chest pain or think you might be having a heart attack, call 911 or your local emergency number. If you don't have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only as a last resort.
Causes
The cause of spontaneous coronary artery dissection is unknown.
Risk factors
Risk factors for SCAD include:
- Female sex. Though SCAD can occur in both men and women, it tends to affect women more than men.
- Childbirth. Some women who have had SCAD have recently given birth. SCAD has been found to occur most often in the first few weeks after delivery, but it can also occur during pregnancy.
- Fibromuscular dysplasia (FMD). This condition, which causes irregular growth of cells in artery walls, can weaken artery walls, leading to blockages, dissections or aneurysms. It can also cause high blood pressure, stroke and tears in other blood vessels. Women are more likely to have FMD than men.
- Hormone use. Hormone therapy, such as from oral contraceptives or infertility treatments, has been associated with SCAD.
- Other conditions affecting blood vessels. Diseases that cause inflammation of the blood vessels, such as lupus and polyarteritis nodosa, also have been associated with SCAD.
- Inherited connective tissue diseases. Genetic diseases that cause problems with the body's connective tissues, such as vascular Ehlers-Danlos syndrome and Marfan syndrome, have been found to occur in people who have had SCAD.
- Very high blood pressure. Severe high blood pressure can be associated with SCAD.
- Illegal drug use. Using cocaine or other illegal drugs might increase the risk of SCAD.
Some episodes of SCAD have occurred after extreme or intense physical exercise and severe emotional stress.
Complications
SCAD is a tear inside an artery that carries blood to the heart. When the inner layers of the artery separate from the outer layers, blood can pool in between the layers. The pressure of the pooling blood can make a short tear longer. Blood trapped between the layers can form a blood clot.
SCAD can slow blood flow through the artery, which weakens the heart muscle. Or blood flow through the artery can stop, causing heart muscle to die (heart attack). A heart attack as a result of SCAD is different from a heart attack caused by hardening of the arteries (atherosclerosis).
SCAD can happen more than once, despite successful treatment, either soon after the first episode or years later. People who have SCAD can also have a higher risk of other heart problems, such as heart failure due to the damage to the heart muscle from heart attacks.
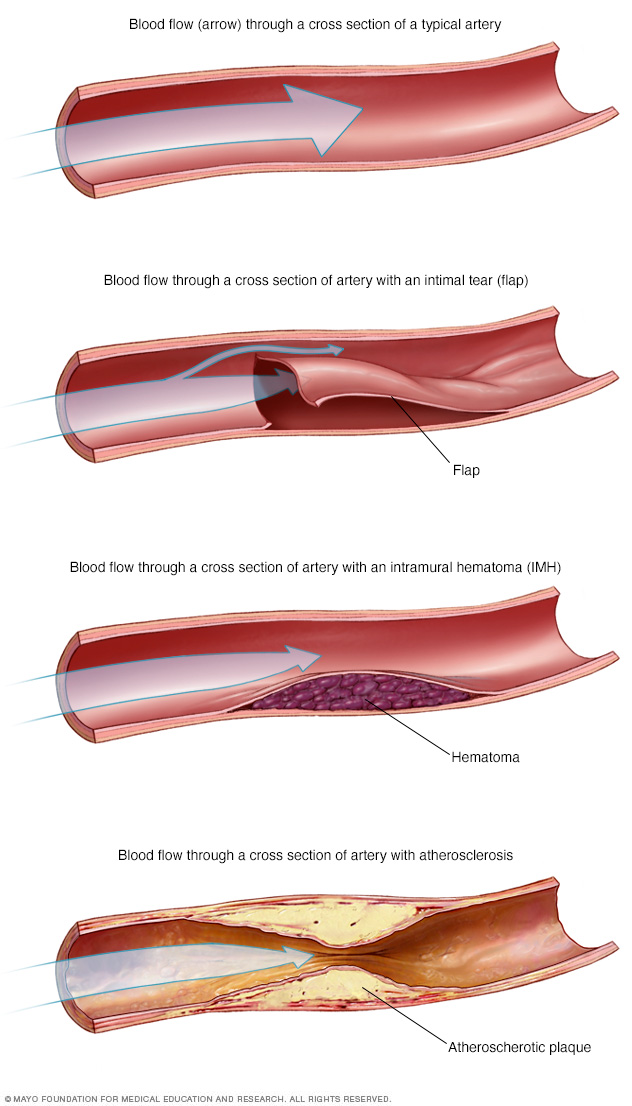
In spontaneous coronary artery dissection (SCAD), a tear forms in an artery in the heart. This can cause blood to pool in the area between the layers. Blood trapped between the layers can form a blood clot (hematoma). SCAD can reduce or block blood flow through the artery, which can cause a heart attack. However, a heart attack as a result of SCAD is different from a heart attack caused by hardening of the arteries (atherosclerosis), shown in the bottom image.
Diagnosis
Tests used to diagnose SCAD, which are similar to those used to evaluate other types of heart attacks, can include:
Coronary angiogram
During a coronary angiogram, a health care provider injects a special dye into the arteries so they'll show up on imaging tests. To get the dye into the arteries, the provider inserts a long, thin tube (catheter) into an artery — usually in the arm or leg — and threads the tube to the arteries in the heart.
Once the dye is released, X-rays are used to create pictures of the arteries. The X-rays can show problems in an artery, which can help confirm SCAD. A coronary angiogram can also show if the arteries in the heart are twisted (tortuous arteries).
Intravascular ultrasound
An intravascular ultrasound test might be done in addition to coronary angiography to help health care providers confirm SCAD and plan treatment. During heart catheterization, a special imaging catheter is passed into the arteries to create pictures using sound waves.
Optical coherence tomography
A catheter equipped with a special light is passed into the arteries to create light-based pictures. This test may be done after coronary angiography.
The optical coherence images can show problems in an artery that can help health care providers confirm a diagnosis of SCAD and gather information to guide treatment.
Cardiac computerized tomography (CT) angiography
During cardiac CT angiography, you usually lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest, which may reveal problems in your arteries.
Cardiac CT angiography might be used with other tests or as a follow-up test to evaluate your condition after SCAD.
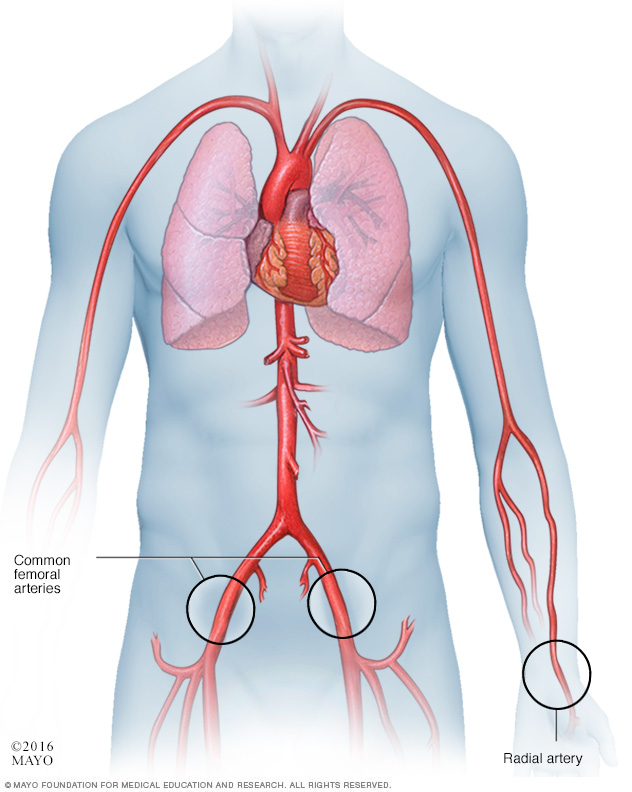
In a cardiac catheter procedure, a health care provider inserts a catheter in an artery in the wrist (radial artery) or in the groin (femoral artery). The catheter is then threaded through the blood vessels to the heart.
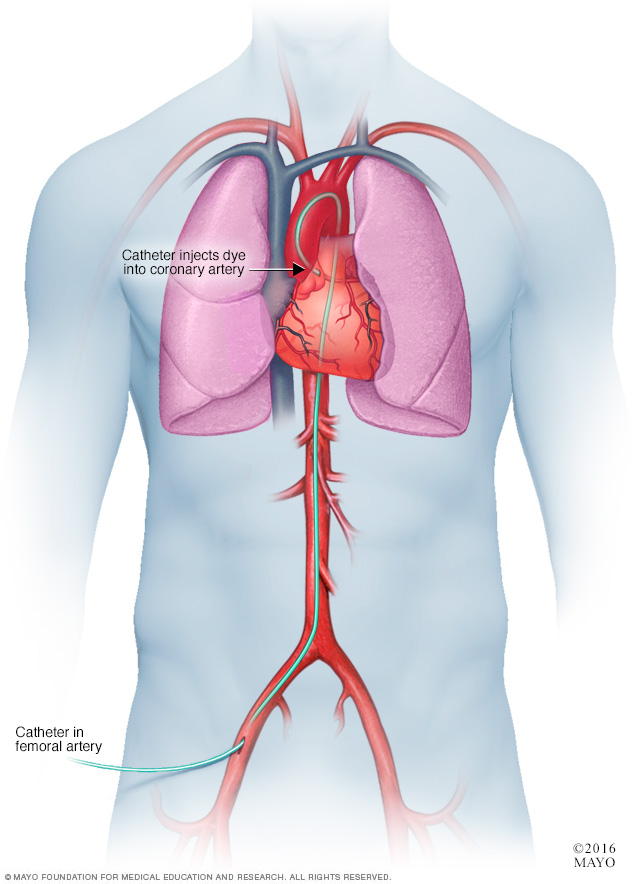
In a coronary angiogram, a catheter is inserted into an artery in the groin, arm or neck and threaded through the blood vessels to the heart. A coronary angiogram can show blocked or narrowed blood vessels in the heart.
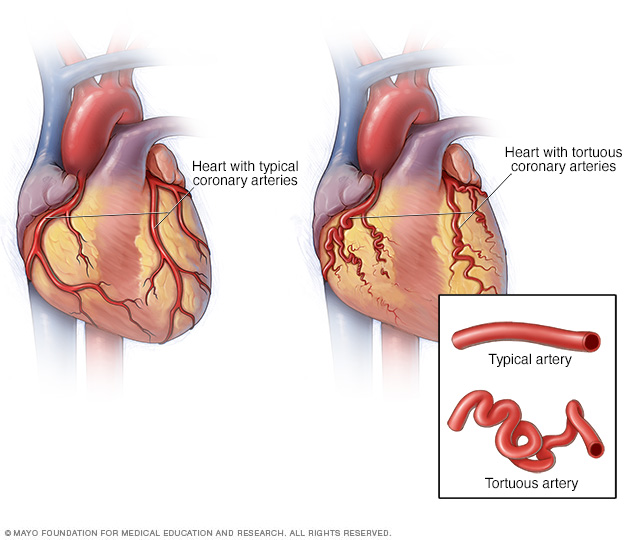
In spontaneous coronary artery dissection (SCAD), the arteries in the heart (coronary arteries) may sometimes be twisted (tortuous arteries).
Treatment
The goal of treatment for SCAD is to restore blood flow to the heart, manage chest pain and prevent recurrence. Sometimes, this healing will occur naturally. Or doctors might have to restore blood flow by opening the artery with a balloon or stent. Bypass surgery also might be used.
The treatments most appropriate for you will depend on your condition, including the size and location of the tear in the artery, as well as your signs or symptoms. Whenever possible, health care providers allow the damaged artery to heal on its own.
For some people, medications might relieve the symptoms of SCAD, so it might be possible to be treated with medications alone. If chest pain or other symptoms persist, other treatments might be needed.
Placing a stent to hold the artery open
If SCAD has blocked blood flow to your heart or if medications don't control your chest pain, your health care provider might recommend placing a tiny mesh tube (stent) inside your artery to hold it open. A stent can help restore blood flow to your heart.
To position the stent, the health care provider inserts a long, thin tube (catheter) into an artery — usually in your leg or arm — and guides the tube to the arteries in your heart. X-rays help the health care provider see where to place the catheter.
A wire with a deflated balloon is passed through the catheter to the tear in the artery. The balloon is then inflated, expanding the stent against your artery walls. The stent is left in place to hold the artery open.
Surgery to bypass the damaged artery
If other treatments haven't worked or if you have more than one tear in an artery, your health care provider might recommend surgery to create a way for blood to reach your heart.
Coronary bypass surgery involves removing a blood vessel from another part of your body, such as your leg. That blood vessel is stitched into place so that it diverts blood flow around your damaged artery.
Medications
After SCAD, your health care provider might recommend medications, including:
- Aspirin. Aspirin might help prevent cardiovascular disease problems after SCAD.
- Blood-thinning drugs. Drugs that reduce the number of blood-clotting platelets in the blood (anticoagulants) can reduce the risk of a clot forming in the torn artery.
- Blood pressure drugs. Drugs used to treat high blood pressure can lower the heart's demand for blood, reducing the pressure in the damaged artery. You might take blood pressure drugs indefinitely to reduce the risk of another SCAD.
- Medications to control chest pain. These medications (nitrates and calcium channel blockers) can help treat chest pain you might have after SCAD.
- Cholesterol drugs. People who have high cholesterol levels and other risk factors might need medications to control their cholesterol levels.
Cardiac rehabilitation
After treatment for SCAD, you'll need regular follow-up appointments with your health care provider to monitor for changes in your condition. Your provider is likely to recommend cardiac rehabilitation.
Cardiac rehabilitation is a customized program of exercise and education that is designed to help you recover from a serious heart condition. The program often includes monitored exercise, nutritional counseling and emotional support.
Coping and support
SCAD can be an unexpected and shocking diagnosis. The condition can cause serious and concerning symptoms, and it often affects people who have few risk factors for heart disease.
To manage the condition, you might try:
Learning more about your diagnosis. Learn about SCAD to feel comfortable talking with your health care provider about your care. Ask about the specifics of your situation, such as the location and size of your artery tear and descriptions of the treatments you've received and where you can find more information.
Women who have had SCAD might be advised to avoid pregnancy.
Take care of yourself. Get enough sleep, eat a healthy diet full of fruits and vegetables, and find ways to manage stress, such as listening to music or keeping a journal.
If you feel anxious or depressed, talk to your health care provider. He or she might recommend that you talk to a mental health professional.
- Be as physically active as you can. If your health care provider agrees, try to do moderate physical activity, such as walking, for 30 to 40 minutes most days of the week. Your health care provider might recommend that you avoid high-intensity activities, competitive or contact sports, or heavy lifting.
- Connect with others living with your diagnosis. SCAD is uncommon, but national organizations can connect you to others who share your diagnosis. Organizations such as the American Heart Association and WomenHeart: The National Coalition for Women with Heart Disease can provide telephone and online support.
Preparing for an appointment
In most cases, SCAD is an emergency situation. If you have chest pain or think that you're having a heart attack, immediately call 911 or your local emergency number.
After your initial diagnosis, you're likely to have questions about your situation. Prepare a list of questions to ask your health care provider at your next visit. Questions you might want to ask include:
- What caused my SCAD?
- What are other possible causes for my symptoms or condition?
- What tests do I need?
- What's the most appropriate treatment?
- Will the tear in my artery heal on its own?
- What is my risk of having another SCAD?
- Do I have blood vessel conditions, such as FMD?
- I have other health conditions. How can I best manage them together?
- Are there any restrictions I need to follow?
- Is it safe for me to get pregnant?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions you have.
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.