Thoracic outlet syndrome (TOS) is a group of disorders that occur when blood vessels or nerves in the space between your collarbone and your first rib (thoracic outlet) are compressed. This can cause shoulder and neck pain and numbness in your fingers.
Common causes of thoracic outlet syndrome include physical trauma from a car accident, repetitive injuries from job- or sports-related activities, certain anatomical defects (such as having an extra rib), and pregnancy. Sometimes doctors don't know the cause of thoracic outlet syndrome.
Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures. Most people improve with these treatments. In some cases, however, your doctor may recommend surgery.
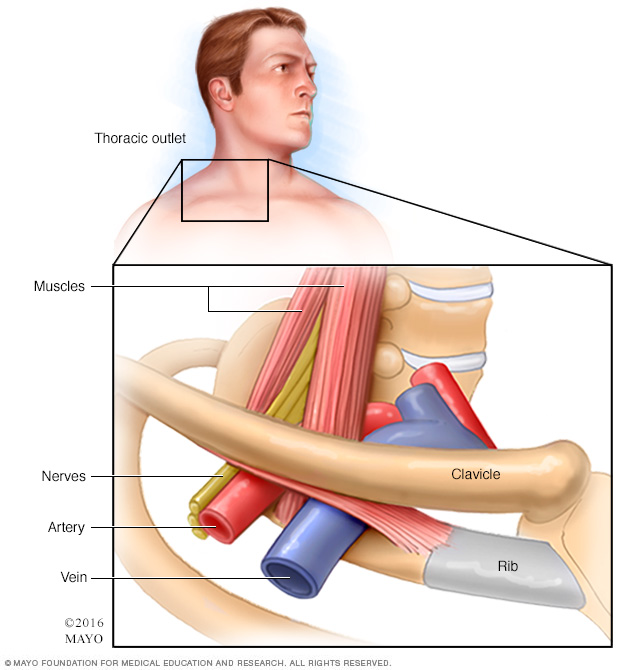
The thoracic outlet is the space between your collarbone (clavicle) and your first rib. This narrow passageway is crowded with blood vessels, nerves and muscles.
Symptoms
There are three general types of thoracic outlet syndrome:
- Neurogenic (neurologic) thoracic outlet syndrome. This most common type of thoracic outlet syndrome is characterized by compression of the brachial plexus. The brachial plexus is a network of nerves that come from your spinal cord and control muscle movements and sensation in your shoulder, arm and hand.
- Venous thoracic outlet syndrome. This type of thoracic outlet syndrome occurs when one or more of the veins under the collarbone (clavicle) are compressed, resulting in blood clots.
- Arterial thoracic outlet syndrome. This is the least common type of TOS. It occurs when one of the arteries under the collarbone is compressed, resulting in bulging of the artery, also known as an aneurysm.
It's possible to have a mix of the three different types of thoracic outlet syndrome, with multiple parts of the thoracic outlet being compressed.
Thoracic outlet syndrome symptoms can vary depending on the type. When nerves are compressed, signs and symptoms of neurogenic thoracic outlet syndrome include:
- Numbness or tingling in your arm or fingers
- Pain or aches in your neck, shoulder, arm or hand
- Weakening grip
Signs and symptoms of venous thoracic outlet syndrome can include:
- Discoloration of your hand (bluish color)
- Arm pain and swelling
- Blood clot in veins in the upper area of your body
- Arm fatigue with activity
- Paleness or abnormal color in one or more fingers or your hand
- Throbbing lump near your collarbone
Signs and symptoms of arterial thoracic outlet syndrome can include:
- Cold fingers, hands or arms
- Hand and arm pain
- Lack of color (pallor) or bluish discoloration (cyanosis) in one or more of your fingers or your entire hand
- Weak or no pulse in the affected arm
When to see a doctor
See your doctor if you consistently experience any of the signs and symptoms of thoracic outlet syndrome.
Causes
Thoracic outlet syndrome is usually caused by compression of the nerves or blood vessels in the thoracic outlet, just under your collarbone (clavicle). The cause of the compression varies and can include:
- Anatomical defects. Inherited defects that are present at birth (congenital) may include an extra rib located above the first rib (cervical rib) or an abnormally tight fibrous band connecting your spine to your rib.
- Poor posture. Drooping your shoulders or holding your head in a forward position can cause compression in the thoracic outlet area.
- Trauma. A traumatic event, such as a car accident, can cause internal changes that then compress the nerves in the thoracic outlet. The onset of symptoms related to a traumatic accident often is delayed.
Risk factors
There are several factors that seem to increase the risk of thoracic outlet syndrome, including:
- Sex. Females are greater than three times more likely to be diagnosed with thoracic outlet syndrome than are males.
- Age. Thoracic outlet syndrome may occur at any age but is most commonly diagnosed in adults between the ages of 20 and 50.
Complications
Complications from this condition stem from the type of presentation (neurogenic, venous or arterial). For patients with venous or arterial TOS, it is important to seek urgent medical attention to make the correct diagnosis and implement appropriate treatment. For neurogenic TOS, it is important to seek medical attention with appropriate evaluation and testing.
Prevention
If you're at risk for thoracic outlet compression, avoid repetitive movements and lifting heavy objects. If you're overweight, losing weight may help you prevent or relieve symptoms of thoracic outlet syndrome.
Even if you don't have symptoms of thoracic outlet syndrome, avoid carrying heavy bags over your shoulder, because this can increase pressure on the thoracic outlet. Stretch daily, and perform exercises that keep your shoulder muscles strong.
Daily stretches focusing on the chest, neck and shoulders can help improve shoulder muscle strength and prevent thoracic outlet syndrome.
Diagnosis
Diagnosing thoracic outlet syndrome can be difficult because the symptoms and their severity can vary greatly among people with the disorder. To diagnose thoracic outlet syndrome, your doctor may review your symptoms and medical history and conduct a physical examination and additional imaging and testing.
- Physical examination. Your doctor will perform a physical examination to look for external signs of thoracic outlet syndrome, such as a depression in your shoulder, a bony abnormality above the collarbone, swelling or pale discoloration in your arm or abnormal pulses. Your doctor may test range of motion and try to reproduce your symptoms by asking you to move or lift your arms or turn your head. Understanding which positions and movements trigger your symptoms can help your doctor identify thoracic outlet syndrome.
- Medical history. Your doctor will likely ask about your medical history and symptoms, as well as your occupation and physical activities.
Imaging and nerve study tests
To confirm the diagnosis of thoracic outlet syndrome, your doctor may order one or more of the following tests:
- Ultrasound. An ultrasound uses sound waves to create images of your body. It's often the first imaging test used to help diagnose thoracic outlet syndrome. Doctors may use this test to see if you have vascular thoracic outlet syndrome or other vascular problems.
- X-ray. Your doctor may order a chest X-ray, which may reveal an extra rib (cervical rib). X-rays can also help to rule out other conditions that could be causing your symptoms.
- Computerized tomography (CT) scan. A CT scan uses X-rays to obtain cross-sectional images of your body. A dye may be injected into a vein to view the blood vessels in greater detail (CT angiography). A CT scan may identify the location and cause of blood vessel (vascular) compression.
- Magnetic resonance imaging (MRI). An MRI uses powerful radio waves and magnets to create a detailed view of your body. Your doctor may use an MRI to determine the location and cause of blood vessel (vascular) compression, sometimes along with an injected dye to better see the blood vessels. An MRI may reveal congenital anomalies, such as a fibrous band connecting your spine to your rib or a cervical rib, which may be the cause of your symptoms. It may be used while your doctor places your head, shoulders and neck in different positions for a better view of the blood vessels in your arm.
-
Arteriography and venography. In these tests, your doctor inserts a thin, flexible tube (catheter) through a small incision, usually in your groin. The catheter is moved through your major arteries in arteriography, or through your veins in venography, to the affected blood vessels. Then your doctor injects a dye through the catheter to show X-ray images of your arteries or veins.
Doctors can check to see if you have a compressed vein or artery. If a vein or artery has a clot, doctors can deliver medications through the catheter to dissolve the clot.
- Electromyography (EMG). During an EMG, your doctor inserts a needle electrode through your skin into various muscles. The test evaluates the electrical activity of your muscles when they contract and when they're at rest. This test can determine if you have nerve damage.
Treatment
In most cases, a conservative approach to treatment may be most effective, especially if your condition is diagnosed early. Treatment may include:
- Physical therapy. If you have neurogenic thoracic outlet syndrome, physical therapy is the first line of treatment. You'll learn how to do exercises that strengthen and stretch your shoulder muscles to open the thoracic outlet, improve your range of motion and improve your posture. These exercises, done over time, may take the pressure off your blood vessels and nerves in the thoracic outlet.
- Medications. Your doctor may prescribe anti-inflammatory medications, pain medications or muscle relaxants to decrease inflammation, reduce pain and encourage muscle relaxation. If there is a blood clot, your doctor may prescribe a blood-thinning medication.
- Clot-dissolving medications. If you have venous or arterial thoracic outlet syndrome and have blood clots, your doctor may administer clot-dissolving medications (thrombolytics) into your veins or arteries to dissolve blood clots. After you're given thrombolytics, your doctor may prescribe medications to prevent blood clots (anticoagulants).
Surgical options
Your doctor may recommend surgery if conservative treatments haven't been effective, if you're experiencing ongoing or worsening symptoms, or if you have progressive neurological problems.
A surgeon trained in chest (thoracic) surgery or blood vessel (vascular) surgery will perform the procedure.
Thoracic outlet syndrome surgery has risks of complications, such as injury to the brachial plexus. Also, surgery may not relieve your symptoms, and symptoms may recur.
Surgery to treat thoracic outlet syndrome, called thoracic outlet decompression, may be performed using several different approaches. These approaches involve removing a muscle and a portion of the first rib to relieve compression. You may also need surgery to repair compressed blood vessels.
In venous or arterial thoracic outlet syndrome, your surgeon may deliver medications to dissolve blood clots prior to thoracic outlet compression. Also, in some cases, your surgeon may conduct a procedure to remove a clot from the vein or artery or repair the vein or artery prior to thoracic outlet decompression.
If you have arterial thoracic outlet syndrome, your surgeon may need to replace the damaged artery with a section of an artery from another part of your body (graft) or an artificial graft. This procedure may be done at the same time as your procedure to have the first rib removed.
Lifestyle and home remedies
If you're diagnosed with thoracic outlet syndrome, your doctor or physical therapist will instruct you to do exercises at home to strengthen and support the muscles surrounding your thoracic outlet.
In general, to avoid unnecessary stress on your shoulders and muscles surrounding the thoracic outlet:
- Maintain good posture
- Take frequent breaks at work to move and stretch
- Maintain a healthy weight
- Create a work area that allows you to keep good posture and doesn't make symptoms worse
- Gently massage your shoulders and thoracic outlet
- Apply a heating pad to the area
- Practice relaxation exercises such as deep breathing, meditation and stretching
Coping and support
Symptoms associated with thoracic outlet syndrome can be caused by a number of other conditions, which makes it difficult for doctors to diagnose the condition. Many people experience thoracic outlet syndrome symptoms for years before they are diagnosed with the condition, which can cause stress and frustration. Be sure to discuss your concerns with your doctor if your symptoms persist and a diagnosis hasn't been made.
Preparing for an appointment
You're likely to start by seeing your primary care doctor. In some cases, your doctor may refer you to a doctor trained in blood vessel (vascular) conditions or blood vessel surgery.
Here's some information to help you prepare for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do before you arrive at the office.
- Write down any symptoms you're experiencing, including any that seem unrelated to the reason for which you scheduled the appointment. Be as specific and detailed as possible in describing your symptoms, including what part of your body is affected and how the discomfort makes you feel.
- Write down key personal information, including any physical traumas you've experienced, such as a car accident or work-related injury. Even if the injuries occurred years ago, your doctor will want to know about them. Also note any repetitive physical activities that you've performed now or in the past at work, in sports, and for hobbies and other recreational activities.
- List your key medical information, including other conditions you're being treated for and the names of any prescription and over-the-counter medications or supplements that you're taking.
- Take a family member or friend along, if possible. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Preparing a list of questions will help you make the most of your time with your doctor. For thoracic outlet syndrome, some basic questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- What kinds of tests do I need?
- What treatments are available, and which treatment do you recommend for me?
- How likely are nonsurgical treatments to improve my symptoms?
- If conservative treatments aren't effective, is surgery an option?
- Is there anything I can do to prevent a recurrence of this problem?
- Will I need to change my job?
- Do I need to limit or give up other activities that may be causing my symptoms?
- If you're recommending weight loss, how much weight do I need to lose to notice an improvement in my symptoms?
- I have other health conditions. How can I best manage them with this condition?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting?
Don't hesitate to ask any other questions you have.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- When did you first notice your symptoms?
- How would you describe your symptoms?
- Have your symptoms changed over time?
- Where does your pain seem to start and where does it go from there?
- Does the pain or numbness worsen when you lift your arms overhead?
- Does anything else seem to worsen or improve your symptoms?
- What activities do you perform on your job?
- Do you or did you play sports?
- What are your hobbies or most frequent recreational activities?
- Have you been diagnosed or treated for any other medical conditions? When?
- Have you noticed a lack of color or a blue color in one or more of your fingers or your entire hand or other changes to the area?
What you can do in the meantime
While you're waiting for your appointment, try taking a nonsteroidal anti-inflammatory drug (NSAID), such as ibuprofen (Advil, Motrin IB, others). Your discomfort may also be improved if you maintain good posture and avoid using repetitive movements and lifting heavy objects.
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.