A transient ischemic attack (TIA) is a temporary period of symptoms similar to those of a stroke. A TIA usually lasts only a few minutes and doesn't cause permanent damage.
Often called a ministroke, a TIA may be a warning. About 1 in 3 people who has a TIA will eventually have a stroke, with about half occurring within a year after the TIA.
A TIA can serve as both a warning of a future stroke and an opportunity to prevent it.
Symptoms
Transient ischemic attacks usually last a few minutes. Most signs and symptoms disappear within an hour, though rarely symptoms may last up to 24 hours. The signs and symptoms of a TIA resemble those found early in a stroke and may include sudden onset of:
- Weakness, numbness or paralysis in the face, arm or leg, typically on one side of the body
- Slurred or garbled speech or difficulty understanding others
- Blindness in one or both eyes or double vision
- Vertigo or loss of balance or coordination
You may have more than one TIA, and the recurrent signs and symptoms may be similar or different depending on which area of the brain is involved.
When to see a doctor
Since TIAs most often occur hours or days before a stroke, seeking medical attention immediately following a possible TIA is essential. Seek immediate medical attention if you suspect you've had a TIA. Prompt evaluation and identification of potentially treatable conditions may help you prevent a stroke.
Causes
A TIA has the same origins as that of an ischemic stroke, the most common type of stroke. In an ischemic stroke, a clot blocks the blood supply to part of the brain. In a TIA, unlike a stroke, the blockage is brief, and there is no permanent damage.
The underlying cause of a TIA often is a buildup of cholesterol-containing fatty deposits called plaques (atherosclerosis) in an artery or one of its branches that supplies oxygen and nutrients to the brain.
Plaques can decrease the blood flow through an artery or lead to the development of a clot. A blood clot moving to an artery that supplies the brain from another part of the body, most commonly from the heart, also may cause a TIA.
Risk factors
Some risk factors for a TIA and stroke can't be changed. Others you can control.
Risk factors you can't change
You can't change the following risk factors for a TIA and stroke. But knowing you're at risk can motivate you to change your lifestyle to reduce other risks.
- Family history. Your risk may be greater if one of your family members has had a TIA or a stroke.
- Age. Your risk increases as you get older, especially after age 55.
- Sex. Men have a slightly higher risk of a TIA and a stroke. But as women age, their risk of a stroke goes up.
- Prior transient ischemic attack. If you've had one or more TIAs, you're much more likely to have a stroke.
- Sickle cell disease. Stroke is a frequent complication of sickle cell disease. Another name for this inherited disorder is sickle cell anemia. Sickle-shaped blood cells carry less oxygen and also tend to get stuck in artery walls, hampering blood flow to the brain. However, with proper treatment of sickle cell disease, you can lower your risk of a stroke.
Risk factors you can control
You can control or treat a number of factors — including certain health conditions and lifestyle choices — that increase your risk of a stroke. Having one or more of these risk factors doesn't mean you'll have a stroke, but your risk increases if you have two or more of them.
Health conditions
- High blood pressure. The risk of a stroke begins to increase at blood pressure readings higher than 140/90 millimeters of mercury (mm Hg). Your health care provider will help you decide on a target blood pressure based on your age, whether you have diabetes and other factors.
- High cholesterol. Eating less cholesterol and fat, especially saturated fat and trans fat, may reduce the plaques in your arteries. If you can't control your cholesterol through dietary changes alone, your provider may prescribe a statin or another type of cholesterol-lowering medication.
- Cardiovascular disease. This includes heart failure, a heart defect, a heart infection or a heart rhythm that isn't typical.
- Carotid artery disease. In this condition, the blood vessels in the neck that lead to the brain become clogged.
- Peripheral artery disease (PAD). PAD causes the blood vessels that carry blood to the arms and legs to become clogged.
- Diabetes. Diabetes increases the severity of atherosclerosis — narrowing of the arteries due to accumulation of fatty deposits — and the speed with which it develops.
- High levels of homocysteine. Elevated levels of this amino acid in the blood can cause the arteries to thicken and scar, which makes them more susceptible to clots.
- Excess weight. Obesity, especially carrying extra weight in the abdominal area, increases stroke risk in both men and women.
- COVID-19. There is evidence that SARS-CoV-2, the virus that causes COVID-19, may raise the risk of stroke.
Lifestyle choices
- Cigarette smoking. Quit smoking to reduce your risk of a TIA and a stroke. Smoking increases your risk of blood clots, raises your blood pressure and contributes to the development of cholesterol-containing fatty deposits in the arteries (atherosclerosis).
- Physical inactivity. Engaging in 30 minutes of moderate-intensity exercise most days helps reduce risk.
- Poor nutrition. Reducing your intake of fat and salt decreases your risk of a TIA and a stroke.
- Heavy drinking. If you drink alcohol, limit yourself to no more than two drinks daily if you're a man and one drink daily if you're a woman.
- Use of illicit drugs. Avoid cocaine and other illicit drugs.
Prevention
Knowing your risk factors and living healthfully are the best things you can do to prevent a TIA. Included in a healthy lifestyle are regular medical checkups. Also:
- Don't smoke. Stopping smoking reduces your risk of a TIA or a stroke.
- Limit cholesterol and fat. Cutting back on cholesterol and fat, especially saturated fat and trans fat, in your diet may reduce buildup of plaques in the arteries.
- Eat plenty of fruits and vegetables. These foods contain nutrients such as potassium, folate and antioxidants, which may protect against a TIA or a stroke.
- Limit sodium. If you have high blood pressure, avoiding salty foods and not adding salt to food may reduce your blood pressure. Avoiding salt may not prevent hypertension, but excess sodium may increase blood pressure in people who are sensitive to sodium.
- Exercise regularly. If you have high blood pressure, regular exercise is one of the few ways you can lower your blood pressure without drugs.
- Limit alcohol intake. Drink alcohol in moderation, if at all. The recommended limit is no more than one drink daily for women and two a day for men.
- Maintain a healthy weight. Being overweight contributes to other risk factors, such as high blood pressure, cardiovascular disease and diabetes. Losing weight with diet and exercise may lower your blood pressure and improve your cholesterol levels.
- Don't use illicit drugs. Drugs such as cocaine are associated with an increased risk of a TIA or a stroke.
- Control diabetes. You can manage diabetes and high blood pressure with diet, exercise, weight control and, when necessary, medication.
Diagnosis
A prompt evaluation of your symptoms is vital in diagnosing the cause of the TIA and deciding on a method of treatment. To help determine the cause of the TIA and to assess your risk of a stroke, your provider may rely on the following:
-
Physical exam and tests. Your provider will perform a physical exam and a neurological exam. The provider will test your vision, eye movements, speech and language, strength, reflexes, and sensory system. Your provider may use a stethoscope to listen to the carotid artery in your neck. A whooshing sound (bruit) may indicate atherosclerosis. Or your provider may use an ophthalmoscope to look for cholesterol fragments or platelet fragments (emboli) in the tiny blood vessels of the retina at the back of the eye.
Your provider may check for risk factors of a stroke, including high blood pressure, high cholesterol levels, diabetes and in some cases high levels of the amino acid homocysteine.
- Carotid ultrasonography. If your provider suspects that the carotid artery may be the cause of your TIA, a carotid ultrasound may be considered. A wand-like device (transducer) sends high-frequency sound waves into the neck. After the sound waves pass through the tissue and back, your provider can analyze images on a screen to look for narrowing or clotting in the carotid arteries.
- Computerized tomography (CT) or computerized tomography angiography (CTA) scanning. CT scanning of the head uses X-ray beams to assemble a composite 3D look at the brain or evaluate the arteries in the neck and brain. CTA scanning uses X-rays similar to a standard CT scan but may also involve injection of a contrast material into a blood vessel. Unlike a carotid ultrasound, a CTA scan can evaluate blood vessels in the neck and head.
- Magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA). These procedures, which use a strong magnetic field, can generate a composite 3D view of the brain. MRA uses technology similar to MRI to evaluate the arteries in the neck and brain but may include an injection of a contrast material into a blood vessel.
-
Echocardiography. Your provider may choose to perform a traditional echocardiography called transthoracic echocardiogram (TTE). A TTE involves moving an instrument called a transducer across the chest. The transducer emits sound waves that bounce off different parts of the heart, creating an ultrasound image.
Or your provider may choose to perform another type of echocardiography called a transesophageal echocardiogram (TEE). During a TEE, a flexible probe with a transducer built into it is placed in the esophagus — the tube that connects the back of the mouth to the stomach.
Because the esophagus is directly behind the heart, clearer, detailed ultrasound images can be created. This allows a better view of some things, such as blood clots, that might not be seen clearly in a traditional echocardiography exam.
-
Arteriography. This procedure gives a view of arteries in the brain not normally seen in X-ray imaging. A radiologist inserts a thin, flexible tube (catheter) through a small incision, usually in the groin.
The catheter is manipulated through the major arteries and into the carotid or vertebral artery. Then the radiologist injects a dye through the catheter to provide X-ray images of the arteries in the brain. This procedure may be used in selected cases.
Treatment
Once your provider has determined the cause of the TIA, the goal of treatment is to correct the issue and prevent a stroke. Depending on the cause of the TIA, your provider may prescribe medication to reduce the tendency for blood to clot or may recommend surgery or a balloon procedure (angioplasty).
Medications
Providers use several medications to decrease the likelihood of a stroke after a TIA. The medication selected depends on the location, cause, severity and type of TIA. Your provider may prescribe:
-
Anti-platelet drugs. These medications make the platelets, one of the circulating blood cell types, less likely to stick together. When blood vessels are injured, sticky platelets begin to form clots, a process completed by clotting proteins in blood plasma.
The most frequently used anti-platelet medication is aspirin. Aspirin is also the least expensive treatment with the fewest potential side effects. An alternative to aspirin is the anti-platelet drug clopidogrel (Plavix).
Your provider might prescribe aspirin and clopidogrel to be taken together for about a month after the TIA. Research shows that taking these two drugs together in certain situations reduces the risk of a future stroke more than taking aspirin alone. There may be certain situations when the duration of taking both medications together may be extended, such as when the cause of the TIA is a narrowing of a blood vessel located in the head.
Alternatively, your provider may prescribe ticagrelor (Brilinta) and aspirin for 30 days to decrease your risk of recurrent stroke.
Your provider may consider prescribing Aggrenox, a combination of low-dose aspirin and the anti-platelet drug dipyridamole, to reduce blood clotting. The way dipyridamole works is slightly different from aspirin.
-
Anticoagulants. These drugs include heparin and warfarin (Jantoven). They affect clotting-system proteins instead of platelet function. Heparin is used for a short time and is rarely used in the management of TIAs.
These drugs require careful monitoring. If atrial fibrillation is present, your doctor may prescribe a direct oral anticoagulant such as apixaban (Eliquis), rivaroxaban (Xarelto), edoxaban (Savaysa) or dabigatran (Pradaxa), which may be safer than warfarin.
Surgery
If you have a moderately or severely narrowed neck (carotid) artery, your provider may suggest carotid endarterectomy (end-ahr-tur-EK-tuh-me). This preventive surgery clears carotid arteries of fatty deposits (atherosclerotic plaques) before another TIA or stroke can occur. An incision is made to open the artery, the plaques are removed and the artery is closed.
Angioplasty
In selected cases, a procedure called carotid angioplasty, or stenting, is an option. This procedure involves using a balloon-like device to open a clogged artery and placing a small wire tube (stent) into the artery to keep it open.
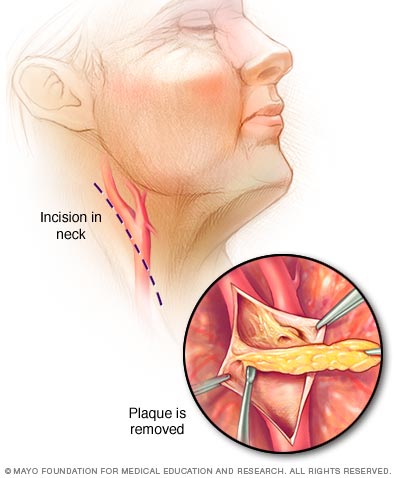
In carotid endarterectomy, your surgeon opens the carotid artery to remove atherosclerotic plaques.
Preparing for an appointment
A TIA often is diagnosed in an emergency situation, but if you're concerned about your risk of having a stroke, you can prepare to discuss the subject with your provider at your next appointment.
What you can do
If you want to discuss your risk of a stroke with your provider, write down and be ready to discuss:
- Your risk factors for a stroke, such as family history of strokes
- Your medical history, including a list of all medications, as well as any vitamins or supplements, you're taking
- Key personal information, such as lifestyle habits and major stressors
- Whether you think you've had a TIA and what symptoms you experienced
- Questions you might have
What to expect from your doctor
Your provider may recommend that you have several tests to check your risk factors. Your provider should tell you how to prepare for the tests, such as fasting before having your blood drawn to check your cholesterol and blood sugar levels.
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.