Truncus arteriosus (TRUNG-kus ahr-teer-e-O-sus) is a rare heart defect that's present at birth (congenital). If you or your baby has truncus arteriosus, it means that one large blood vessel leads out of the heart. Normally, there are two separate vessels coming out of the heart.
In addition, there is usually a hole — known as a ventricular septal defect — between the two lower chambers of the heart. As a result of truncus arteriosus, oxygen-poor blood that should go to the lungs and oxygen-rich blood that should go to the rest of the body are mixed. This creates severe circulatory problems.
Untreated, truncus arteriosus can be fatal. Surgery to repair truncus arteriosus is generally successful, especially if the repair occurs before your baby is 1 month old.
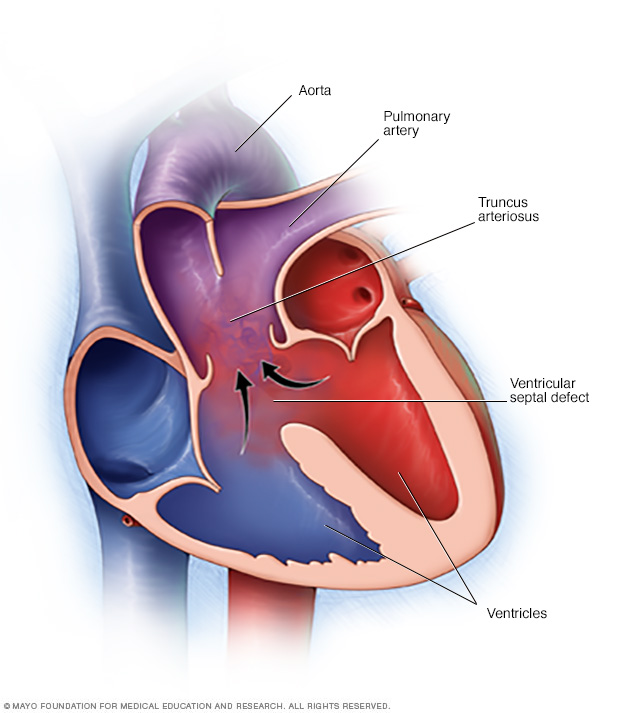
If you or your baby has truncus arteriosus, one large vessel leads out of the heart, instead of two separate vessels, and there's a hole in the wall between the ventricles (ventricular septal defect). The oxygen-rich blood (red) and the oxygen-poor blood (blue) mix together, resulting in blood with an insufficient oxygen supply (purple) for the body.
Symptoms
Signs and symptoms of truncus arteriosus often develop in the first few days of life. They include:
- Blue coloring of the skin
- Poor feeding
- Pounding heart
- Excessive sleepiness
- Poor growth
- Shortness of breath
- Rapid breathing
When to see a doctor
Seek medical treatment if you notice that your baby has any of the following problems:
- Blue coloring of the skin (cyanosis)
- Poor feeding
- Excessive sleepiness
Some signs of truncus arteriosus can indicate a problem that needs urgent care. If your baby has any of the following signs and symptoms and you can't see your baby's doctor immediately, seek emergency medical care:
- Rapid, shallow or labored breathing
- Worsening of blue coloring of the skin
- Loss of consciousness
Causes
Truncus arteriosus occurs when your baby's heart is developing in the womb, and is, therefore, present at birth (congenital). In most cases the cause is unknown.
The heart
Your heart has four pumping chambers that circulate your blood. The "doors" of the chambers (valves) control the flow of blood, opening and closing to ensure that blood flows in a single direction.
The heart's four chambers are:
- The right atrium, the upper right chamber, receives oxygen-poor blood from your body and delivers it into the right ventricle.
- The right ventricle, the lower right chamber, pumps the blood through a large vessel called the pulmonary artery and into the lungs, where the blood is resupplied with oxygen.
- The left atrium, the upper left chamber, receives the oxygen-rich blood from the lungs and delivers it into the left ventricle.
- The left ventricle, the lower left chamber, pumps the oxygen-rich blood through a large vessel called the aorta and on to the rest of the body.
Normal heart development
The formation of the fetal heart is complex. At a certain point, all babies have a single large vessel (truncus arteriosus) exiting the heart. During normal development of the heart, however, this very large single vessel divides into two parts.
One part becomes the lower portion of the aorta, which is attached to the left ventricle. The other part becomes the lower portion of the pulmonary artery, which is attached to the right ventricle.
Also during this process, the ventricles develop into two chambers separated by a wall (septum).
Truncus arteriosus in newborns
In babies born with truncus arteriosus, the single large vessel never finished dividing into two separate vessels and the wall separating the two ventricles never closed completely, resulting in a single blood vessel arising from the heart, and a large hole between the two chambers (ventricular septal defect).
In addition to the primary defects of truncus arteriosus, the valve controlling blood flow from the ventricles to the single large vessel (truncal valve) is often defective, so that it does not close completely, allowing blood to flow backward into the heart.
Risk factors
While the exact cause of congenital heart defects, such as truncus arteriosus, is unknown, several factors might increase the risk of a baby being born with a heart condition. These include:
- Viral illness during pregnancy. If a woman contracts rubella (German measles) or another viral illness during early pregnancy, the risk of congenital heart defects in her baby is increased.
- Poorly controlled diabetes during pregnancy. Diabetes that isn't well-managed can increase the risk of birth defects, including heart defects.
- Certain medications taken during pregnancy. Many medications aren't recommended for use during pregnancy because of potential risks to the fetus.
- Certain chromosomal disorders. Children with DiGeorge's syndrome or velocardiofacial syndrome have an increased risk of truncus arteriosus. These conditions are caused by an extra or defective chromosome.
- Smoking during pregnancy. Continuing to smoke while pregnant increases the risk that the baby will be born with a heart defect.
- Alcohol use. Women who drink alcohol during the first trimester of pregnancy increase their risk of having a baby with a congenital heart defect. Men who drink alcohol also contribute to their baby's congenital heart defect risk.
- Obesity. Women who are obese can have an increased risk of having babies with congenital heart defects.
Complications
The abnormal heart structures of truncus arteriosus result in severe problems with blood circulation.
Because the ventricles aren't separated and all blood exits from a single vessel, the oxygen-rich blood and the oxygen-poor blood mix — resulting in blood that doesn't carry enough oxygen. The mixed blood flows from the single large vessel to the lungs, the arteries of the heart and the rest of the body.
If your baby has truncus arteriosus, the abnormal circulation of blood usually results in:
- Respiratory problems. Too much blood flows into the lungs, and the excess fluid makes it difficult for your baby to breathe.
- High blood pressure in the lungs (pulmonary hypertension). Increased blood flow to the lungs causes the lungs' blood vessels to narrow, increasing blood pressure in the lungs and making it increasingly difficult for your baby's heart to pump blood into the lungs.
- Enlargement of the heart (cardiomegaly). Pulmonary hypertension and the increased blood flow through the heart force your baby's heart to work harder than normal, causing it to enlarge. The enlarged heart gradually weakens.
- Heart failure. The increased workload and poor oxygen supply also result in weakening of your baby's heart. These factors can contribute to heart failure, the inability of the heart to supply the body with enough blood.
Complications later in life
Even with successful surgical repair of the heart during infancy, other complications associated with truncus arteriosus can occur later in life:
- Progressive pulmonary hypertension
- Leaky heart valves (regurgitation)
- Heart rhythm disturbances (arrhythmias)
- Problems related to prior operation
Common signs and symptoms of these complications include shortness of breath when exercising, dizziness, fatigue, abdominal swelling, swelling in the legs and feet, and a sensation of rapid, fluttering heartbeats (palpitations).
Truncus arteriosus in adults
In rare cases, a person with truncus arteriosus can survive infancy without surgical repair of the heart and live into adulthood. However, people with this condition will almost certainly develop heart failure and pulmonary hypertension (Eisenmenger syndrome).
This syndrome is caused by permanent lung damage from pulmonary hypertension that results in much of the blood flow bypassing the lungs entirely.
Prevention
In most cases, congenital heart defects such as truncus arteriosus can't be prevented. If you have a family history of heart defects or if you already have a child with a congenital heart defect, you and your partner might consider talking with a genetic counselor and a cardiologist experienced in congenital heart defects before you make a decision about becoming pregnant.
If you're thinking about becoming pregnant, there are several steps you can take to help ensure a healthy baby, including:
- Getting vaccinated before getting pregnant. Certain viruses, such as German measles (rubella), can be harmful during pregnancy, so it's important to make sure your immunizations are up to date before you get pregnant.
- Avoiding dangerous medications. Check with your doctor before taking any medications if you're pregnant or thinking about becoming pregnant. Many drugs aren't recommended for use during pregnancy.
- Taking folic acid. One of the few steps you can take to help prevent birth defects, including spinal cord, brain and possibly heart defects, is to take 400 micrograms of folic acid daily.
- Controlling diabetes. If you're a woman with diabetes, talk to your doctor about pregnancy risks associated with diabetes and how best to manage the disease during your pregnancy.
Diagnosis
Your baby's doctor will listen to your or your baby's lungs to assess his or her breathing and the possibility of fluid in the lungs. The doctor will listen to your or your baby's heart to determine if there are irregular heartbeats (arrhythmia) or an abnormal sound caused by turbulent blood flow (heart murmur).
For babies with truncus arteriosus, much of their medical care is provided by a pediatric cardiologist along with a pediatric cardiac surgeon and often a team of specialized staff. For adults with truncus arteriosus, much of their medical care is provided by an adult congenital cardiologist along with a congenital cardiac surgeon and often a whole team of specialized staff.
For the pediatric or adult congenital cardiologist to check the condition of your or your baby's heart and make a diagnosis, he or she will order one or more tests:
-
Echocardiogram. An echocardiogram shows the structure and function of the heart. A transducer that emits sound waves is moved across the skin over the heart. The sound waves echo off internal structures, producing images on a monitor.
In a baby with truncus arteriosus, the echocardiogram reveals the single large vessel leading from the heart, a hole in the wall between the left and right ventricles, and abnormalities in the valve between the large vessel and the ventricles. The test can also show how much blood is flowing to your baby's lungs, and whether there's a risk of high blood pressure in the lungs.
- X-ray. An X-ray uses radiation to produce still images of internal organs and structures. A chest X-ray can show the size of the heart, abnormalities in the lungs and excess fluid in the lungs.
Treatment
Infants with truncus arteriosus must have surgery. Multiple procedures or surgeries might be necessary, especially as your child grows. Medications might be given before surgery to help improve heart health.
Children and adults with surgically repaired truncus arteriosus must have regular follow-up with their cardiology team.
Medications
Medications that might be prescribed before surgery include:
- Diuretics. Often called water pills, diuretics increase the frequency and volume of urination, preventing fluid from collecting in the body, which is a common effect of heart failure.
- Inotropic agents. This type of medication strengthens the heart's contractions.
Surgical procedures
Most infants with truncus arteriosus have surgery within the first few weeks after birth. The procedure will depend on your baby's condition. Most commonly your baby's surgeon will:
- Close the hole between the two ventricles with a patch
- Separate the upper portion of the pulmonary artery from the single large vessel
- Implant a tube and valve to connect the right ventricle with the upper portion of the pulmonary artery — creating a new, complete pulmonary artery
- Reconstruct the single large vessel and aorta to create a new, complete aorta
After corrective surgery, your child will need lifelong follow-up care with a cardiologist. The cardiologist might recommend that your child limit physical activity, particularly intense competitive sports.
Your child will need to take antibiotics before dental procedures and other surgical procedures to prevent infections.
Because the artificial conduit does not grow with your child, follow-up surgeries to replace the conduit valve are necessary as he or she ages.
Cardiac catheterization
Minimally invasive procedures use a cardiac catheter to avoid the need for traditional heart surgery as your child grows or previously placed artificial valves deteriorate. The catheter is inserted into a blood vessel in the leg that is then threaded up to the heart to replace the conduit.
In addition, cardiac catheterization with an inflatable balloon tip can be used to open up an obstructed or narrowed artery, which might delay the need for follow-up surgery.
Pregnancy
Women who've had surgery to repair truncus arteriosus in infancy need to be evaluated by a cardiologist with expertise in adult congenital heart defects and an obstetrician specializing in high-risk pregnancies before attempting to become pregnant.
Depending on the level of lung damage that occurred before surgery, pregnancy might or might not be recommended. In addition, some drugs taken for heart problems can be harmful to an unborn baby.
Coping and support
Caring for a baby with a serious heart problem, such as truncus arteriosus, can be challenging. Here are some strategies that may help make it easier:
- Seek support. Ask for help from family members and friends. Contact nonprofit organizations, such as the American Heart Association, Adult Congenital Heart Association or Mended Hearts for information about support groups in your area.
-
Record your baby's health history. Write down your baby's diagnosis, medications, surgery and other procedures, the dates they were performed, your pediatric cardiologist's name and phone number, and other important information about your baby's care.
It's also helpful to include a copy of the operative report from your child's surgeon in your records. This information will help you recall the care your child has received and be useful to doctors unfamiliar with your child who need to review his or her health history. It will also be helpful when your child moves from pediatric to adult health care.
-
Talk about your concerns. You might worry about the risks of vigorous activity, even after your child has had corrective surgery. Talk with the cardiologist about which activities are safe for your child.
If some activities are off-limits, encourage your child in other pursuits rather than focusing on what he or she can't do. If other issues about your child's health concern you, discuss them with your child's primary care doctor or pediatric cardiologist.
Preparing for an appointment
What you can do
If possible, compile a thorough medical history from both sides of your baby's family. Some heart problems are inherited, so it's helpful if you can let your doctor know if anyone in your child's family has ever had early heart problems.
It's also helpful to prepare a list of questions so that you can make the most of your time with your baby's doctor. Here's a sampling of questions you might want to ask:
- What kinds of tests will my child undergo?
- What are the options for treatment? What are the possible complications of treatment?
- What is the long-term outlook for my child?
- What impact would a heart defect or the subsequent treatment have on another condition my baby has?
- If I have another baby in the future, what are the chances of this happening again?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your child's doctor will likely ask you the following questions:
- Does your baby ever appear blue?
- How long are feeding times, or how much does your baby drink?
- How often and how long does your baby sleep?
- How does your baby respond to touch?
- Have you noticed changes in any of these behaviors?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.