What is COVID-19?
COVID-19 is a disease that was identified in December 2019 in Wuhan, China, after a number of people there were reported to have experienced an unusual pneumonia. The disease is caused by a new type of coronavirus, which the World Health Organization (WHO) has called SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2).
The exact beginning of the outbreak of this virus is unclear, but experts estimate it started somewhere between mid-November and December 1, 2019. It is believed that the virus responsible for causing this disease may have passed from bats, potentially through another animal species, to the first individuals before human-to-human transmission became established.
What causes COVID-19?
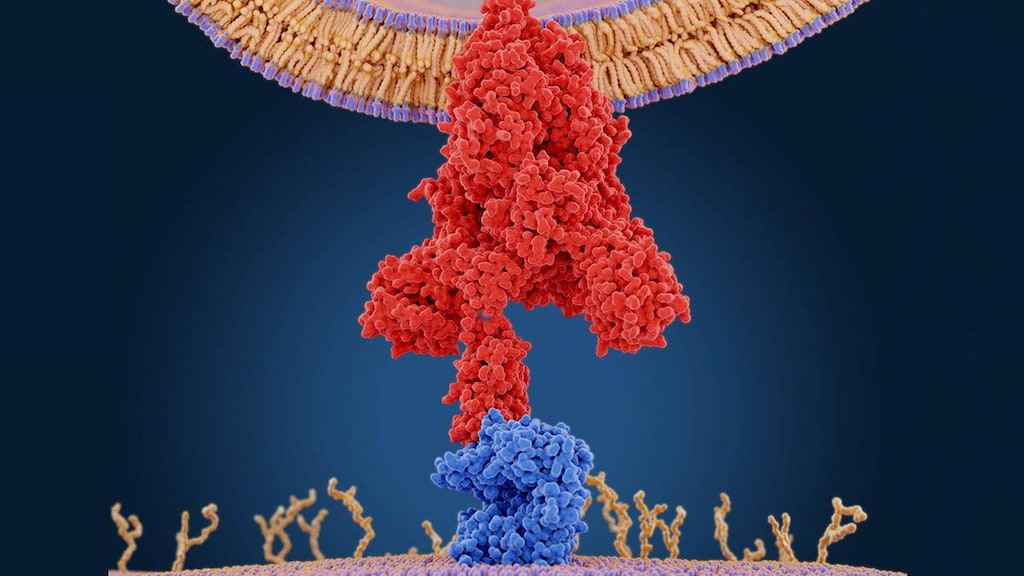
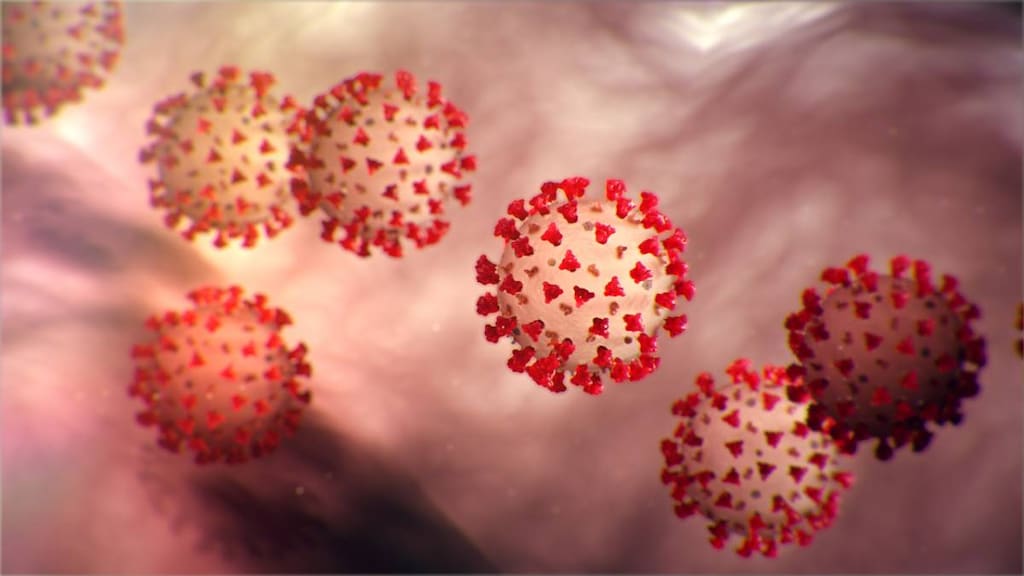
COVID-19 is caused by a coronavirus called SARS-CoV-2. Coronaviruses are enveloped positive-strand RNA viruses named for the large spikes on their surface that look like a crown, which is called a corona in Latin. SARS-CoV-2 belongs to the Coronaviridae family of coronaviruses and is part of the species severe acute respiratory syndrome-related coronavirus, one of 39 species of coronaviruses that had been identified by March 2020.
SARS-CoV-2 targets angiotensin-converting enzyme 2 (ACE2), which is a protein found on the surface of certain cells deep in the airways. By binding to ACE2 receptors the virus is able to enter the cells and cause an infection. ACE2 is the same receptor targeted by another coronavirus called SARS, which caused an epidemic in 2003. Coronaviruses are also responsible for MERS (Middle East respiratory syndrome) and even some common colds.
SARS-CoV-2 is:
- Primarily spread from person to person via infected respiratory droplets that are released when a person with COVID-19 coughs, sneezes or exhales. Droplets are most likely to infect others in close proximity (within 6 feet).
- Potentially picked up from infected surfaces if you touch the surface and then touch your face, nose or eyes. The virus can live on surfaces for hours to days, lasting for longer periods of time on stainless steel and plastic compared with copper and cardboard.
- Being investigated for its potential to spread via aerosols (very small droplets) through the air. Results suggest that potentially infectious aerosols containing SARS-CoV-2 may be able to linger in the air for up to 16 hours, which is of particular concern in crowded spaces with little air flow.
People infected with SARS-CoV-2 are thought to be most infectious in the days before they develop symptoms (pre-symptomatic phase) and at the time their symptoms begin. Initial reports indicated that a person with COVID-19 was likely to infect 2-3 others, but subsequent analysis suggests that the real figure could be as high as 5.7 (R0 = 5.7). COVID-19 is more infectious that influenza (flu), but less infectious that measles, which has an R0 of 12-18.
What are the symptoms of COVID-19?
Common symptoms of COVID-19 include:
- Fever
- A new continuous dry cough
- Fatigue
- Shortness of breath
- Digestive symptoms - including loss of appetite and diarrhea
- Loss of sense of smell and taste
- Pneumonia
Muscle and joint aches and pains, sore throats, headaches and chills are also symptoms of COVID-19. Other less common symptoms include nausea and vomiting, nasal congestion and sneezing, coughing up blood and conjunctivitis.
Initially thought of as a type of viral respiratory pneumonia, COVID-19 is now known to have a widespread effect throughout the body. It is thought to cause inflammation-inducing blood clots that result in a range of complications including heart, lung and kidney injury, as well as strokes and other issues.
In March 2020, the director of the US Centers for Disease Control and Prevention (CDC), also reported that as many as 25% of those with COVID-19 may not show any symptoms, which is known as being asymptomatic. There is still some uncertainty, however, regarding exactly how many people are likely to be truly asymptomatic rather than just pre-symptomatic.
How is COVID-19 diagnosed?
COVID-19 is diagnosed following a positive test for SARS-CoV-2. The testing process typically involves taking a swab of the mouth, throat or back of the nose, which is then checked for signs of the virus using a RT-PCR (reverse transcription polymerase chain reaction) test. This test multiples copies of any genetic material on the sample, so that the virus can be detected.
It is possible to have a negative test result even when you have COVID-19. This can be due to the swab not collecting any virus fragments or because the sample was stored incorrectly before it was tested. Positive test results are also possible even when you are no longer infectious and this is possible because it takes time for the cells in the airways, which may contain dead fragments of the virus, to die off and be replaced (cell turnover). The RT-PCR test does not distinguish between live and dead virus fragments - it will multiply copies of both.
Probable or suspected cases of COVID-19 may also be diagnosed by taking into account a person's symptoms and history of potential exposure to others with COVID-19.
How is COVID-19 treated?
Mild cases of COVID-19 can be treated at home with the help of common over-the-counter medications such as acetaminophen (Tylenol) and ibuprofen (Advil, Motrin IB).
More severe cases requiring hospital admission may receive:
- Supportive treatment, such as oxygen and fluid replacement
- Low molecular weight heparin to prevent blood clots
- Antibiotics to prevent a secondary bacterial infection
- Antivirals approved for other viral illnesses
- Remdesivir, which is available via a Food and Drug Administration (FDA) Emergency Use Authorization (EUA) for patients hospitalized with COVID-19. Remdesivir is an experimental nucleotide analog, which works by blocking an enzyme necessary for viral replication.
- Other experimental treatments such as Baricitinib (Olumiant), Tocilizumab (Actemra) and others.
What is the prognosis for COVID-19?
About 80% of people infected with SARS-CoV-2 are thought to experience mild-to-moderate COVID-19 symptoms. However, 13.8% and 6.1% of people will experience severe or critical symptoms of the disease, respectively. A total of 88% of patients requiring invasive mechanical ventilation died, according to the results of one study in New York, compared with 53% of patients in a UK study.
On May 4, 2020, the WHO estimated the overall global case fatality rate (CFR) to be 7%. This figure represents the total number of deaths reported divided by the total number of infections reported. The CFR varies widely from country to country and is affected by a number of factors. During a pandemic the CFR tends to start off high and then trend downwards. The infection fatality rate (IFR), which is the proportion of deaths among all infected people including confirmed, probable, asymptomatic and undiagnosed cases, is estimated to be 0.01-0.5% depending on the country.
COVID-19 risk factors
People most at risk from COVID-19 include:
- People aged 65 years of age or older
- People with underlying health conditions including those with:
- High blood pressure (hypertension)
- Obesity
- Diabetes
- Cardiovascular or cerebrovascular disease
- Respiratory disease
- Men
- Smokers
In a US Centers for Disease Control and Prevention (CDC) report looking at COVID-19 patients hospitalized during March 2020, high blood pressure was the most common underlying condition reported in older COVID-19 patients, while the most common underlying condition observed in those less than 65 years old was obesity. In a New York study, severe obesity (BMI or body mass index >40) was the second most common predictor of hospitalization after age, with those over 75 years of age being most at risk. The researchers also found that patients with signs of inflammation were among those most likely to become critically ill.
How is COVID-19 prevented?
Vaccines to prevent SARS-CoV-2 infection and the development of COVID-19 are currently underway, with clinical development of some candidates having already begun.
The CDC also recommends the following steps to help prevent the spread of COVID-19:
-
Stay at home as much as possible and avoid close contact with others
-
Practice social distancing and wear a mask when you go out
-
Wash your hands
-
Cover coughs and sneezes with a tissue or the inside of your elbow
-
Clean and disinfect surfaces you touch often such as door handles, counter tops, taps, phones and keyboards for example
Article references
- World Health Organization (WHO). Naming the coronavirus disease (COVID-19) and the virus that causes it. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. [Accessed May 5, 2020].
- World Health Organization (WHO). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). February 16-24, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. [Accessed May 5, 2020].
- Hoffmann M, Kleine-Weber H, Kruger N et al. January 31, 2020. The novel coronavirus 2019 (2019-nCoV) uses the SARS-coronavirus receptor ACE2 and the cellular protease TMPRSS2 for entry into target cells. bioRxiv doi: https://doi.org/10.1101/2020.01.31.929042. [Accessed May 5, 2020].
- Letko M, Munster V. January 22, 2020. Functional assessment of cell entry and receptor usage for lineage B β coronaviruses, including 2019-nCoV. bioRxiv 2020.01.22.915660; doi: 10.1101/2020.01.22.915660. [Accessed May 5, 2020].
- Gorbalenya AE, Baker SC, Baric RS, et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol 5, 536–544 (2020). https://doi.org/10.1038/s41564-020-0695-z.
- van Doremalen N, Bushmaker T, Morris DH. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. April 16, 2020. N Engl J Med 2020; 382:1564-1567. DOI: 10.1056/NEJMc2004973.
- Fears AC, Kilmstra WB, Duprex P, et al. Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol suspensions. medRxiv. April 18, 2020. doi: https://doi.org/10.1101/2020.04.13.20063784. [Accessed May 5, 2020].
- Centers for Disease Control and Prevention (CDC). Presymptomatic Transmission of SARS-CoV-2 - Singapore, January 23-March 16, 2020. Weekly / April 10, 2020 / 69(14);411–415. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e1.htm. [Accessed May 5, 2020].
- He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. April 15, 2020. https://doi.org/10.1038/s41591-020-0869-5.
- New York Times. Infected but Feeling Fine: The Unwitting Coronavirus Spreaders. March 31, 2020. Available at: https://www.nytimes.com/2020/03/31/health/coronavirus-asymptomatic-transmission.html. [Accessed May 5, 2020].
- Centers for Disease Control and Prevention (CDC). High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg Infect Dis. 2020 Jul. https://doi.org/10.3201/eid2607.200282. Accessed May 5, 2020].
- Guerra FM, Bolotin S, Lim G, et al. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017 Dec;17(12):e420-e428. DOI:https://doi.org/10.1016/S1473-3099(17)30307-9.
- BMJ Best Practice. Coronavirus disease 2019 (COVID-19). Prognosis. Available at: https://bestpractice.bmj.com/topics/en-gb/3000168/prognosis. [Accessed May 5, 2020].
- World Health Organization (WHO). Q&A: Similarities and differences – COVID-19 and influenza. March 17, 2020. Available at: https://www.who.int/news-room/q-a-detail/q-a-similarities-and-differences-covid-19-and-influenza. [Accessed May 5, 2020].
- US Food & Drug Administration (FDA). Emergency Use Authorization (EUA) letter for remdesivir. May 1, 2020. Available at: https://www.fda.gov/media/137564/download. [Accessed May 5, 2020].
- American Society of Hematology. COVID-19 and VTE/Anticoagulation: Frequently Asked Questions. April 17, 2020. Available at: https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation. [Accessed May 5, 2020].
- Centers for Disease Control and Prevention (CDC). Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 - COVID-NET, 14 States, March 1-30, 2020. April 17, 2020. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e3.htm?s_cid=mm6915e3_w. [Accessed May 5, 2020].
- Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospitalization and critical illness among 4,103 patients with Covid-19 disease in New York City. medRxiv preprint. April 11, 2020. doi: https://doi.org/10.1101/2020.04.08.20057794. [Accessed May 5, 2020].
- World Health Organization (WHO). DRAFT landscape of COVID-19 candidate vaccines – 11 April 2020. April, 11, 2020. Available at: https://www.who.int/blueprint/priority-diseases/key-action/Novel_Coronavirus_Landscape_nCoV_11April2020.PDF?ua=1. [Accessed May 5, 2020].
- Centers for Disease Control and Prevention (CDC). Coronavirus Disease 2019 (COVID-19). Protect Yourself. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. [Accessed May 5, 2020].