Why Do More Men Die Of COVID-19


We are all human, but we are all different.
Sure, we have many similarities – two eyes, one mouth, two arms, two legs; the list could go on forever.
But we have even more differences. Three million base pairs to be exact (base pairs are the building blocks of our DNA).
Some of these differences are obvious, such as our eye, hair, or skin color. But many more aren’t. And it’s the not-so-obvious genetic differences that can make the biggest impact. For example, losing your hair, or not; developing cancer, or not; and now it seems, dying from COVID-19, or not.
Scientists are still struggling to understand many features of this novel coronavirus – such as how easily it spreads and the best way to treat it. But there is an abundance of data emerging that shows some people are definitely more susceptible than others to severe COVID-19 symptoms.
Men and COVID-19
Being a man is one. 73% of people admitted to an ICU in Wuhan with severe symptoms of COVID-19 were men. Other studies collaborate these statistics, with the reports out from China indicating at least a 12% higher incidence rate and a 25% to 40% higher fatality rate in men.
This is not the first time that men have appeared more susceptible to a viral infection. Both Middle Eastern Respiratory Syndrome (MERS; identified in 2012) and Severe Acute Respiratory Syndrome (SARS; identified in 2003), also types of coronavirus, disproportionately infected men.
Experts aren’t sure exactly what it is about being male that makes them more likely to be infected as well as develop severe symptoms. Perhaps it is that men are more likely to have conditions such as heart disease or diabetes at a younger age, which increases their risk. Maybe it’s hormonal differences that compromise the robustness of a man’s immune system or is it because estrogen has a protective effect for women? Or could it be because more men smoke?
Smoking and COVID-19
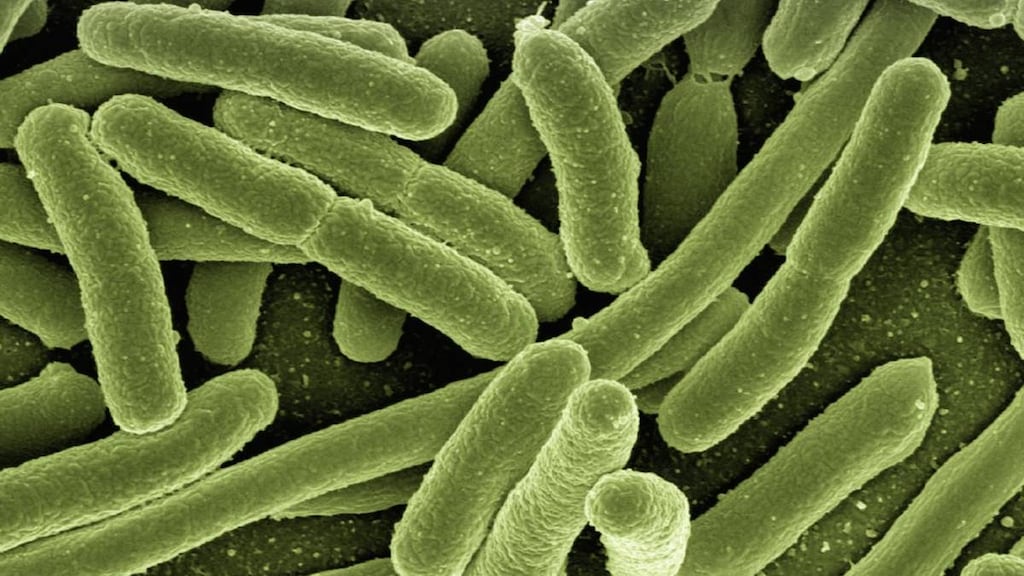
Smoking is associated with a higher risk of developing pneumonia from the virus. Smoking suppresses the way our immune system reacts to bacteria, and research shows smokers are three times more likely than nonsmokers to develop pneumonia – regardless of what respiratory virus they are exposed to.
Age and COVID-19
Older people are also more at risk of severe symptoms. Nearly 50% of those over the age of 65 with COVID-19 required ICU admission and nearly 10% died. Other factors that have shown to increase the risk of death include underlying medical conditions, such as diabetes, high blood pressure, heart disease, or gastrointestinal disease.
Could a common blood pressure medicine affect coronavirus?
Experts have discovered that the main entry point of the coronavirus in humans is via ACE-2 receptors in the lungs. Both MERS and SARS gained entry through these receptors as well.
ACE-2 receptors are a type of protein located on the inner surface of our lungs and are also found in other parts of our body, such as our heart, kidneys, and within our digestive system. ACE-2 receptors control the production of ACE, an enzyme that is part of a wider system that has many vital roles in the body, one of which is the regulation of blood pressure. You may have heard of ACE inhibitors, such as enalapril and lisinopril, which are used for the treatment of high blood pressure. These work by inhibiting the ACE enzyme.
This has got experts thinking. What if we had a medicine that could either block this ACE-2 receptor or saturate it to prevent the entry of this new coronavirus (and any other future coronaviruses for that matter)? Would that stop the infection?
It may prove to be another way to treat the virus, but at the moment, research is still ongoing.
Meanwhile, the American Heart Association (AHA), the Heart Failure Society of America and the American College of Cardiology (ACC) recommend continuation of angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blocker (ARB) medications for all patients already prescribed those drugs for heart failure, high blood pressure or heart disease.
People with heart disease are already at higher risk for symptoms of COVID-19, and it is important to follow the advice of your physician. Examples of ACE inhibitors include enalapril (Vasotec), captopril (Capoten), and lisinopril (Zestril). ARBs include losartan (Cozaar), olmesartan (Benicar) and telmisartan (Micardis) and researchers are thinking they could provide another way to curb the spread of coronavirus.
Article references
- Huang C, Wang Y, Xingwang L et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. January 24, 2020. Lancet 2020; 395: 497–506. doi:https://doi.org/10.1016/S0140-6736(20)30183-5
- Yang Y, Lu Q, Mingjin L et al. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China medRxiv doi: https://doi.org/10.1101/2020.02.10.20021675 [Accessed February 19, 2020].
- Chinese Report Says Lion's Share of Coronavirus Cases Are Mild. Drugs.com News https://www.drugs.com/news/chinese-report-says-lion-s-share-coronavirus-cases-mild-88357.html [Accessed February 19, 2020].
- Smokers at increased risk of coronavirus complications, leading experts warn. Feb 14, 2020. The Telegraph. https://www.telegraph.co.uk/global-health/science-and-disease/coronavirus-dangerous-smokers/ [Accessed February 19, 2020].
- Jia HP, Look DC, Shi L, et al. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J Virol. 2005;79(23):14614–14621. doi:10.1128/JVI.79.23.14614-14621.2005
- Zhao Y, Zhao Z, Wang Y et al. January 26, 2020. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. bioRxiv doi: https://doi.org/10.1101/2020.01.26.919985 [Accessed February 19, 2020].
- Phadke MA, Saunik S. Response to the emerging novel coronavirus outbreak. January 31, 2020. BMJ 2020;368. doi: https://doi.org/10.1136/bmj.m406 [Accessed February 19, 2020].