What is prostate cancer?
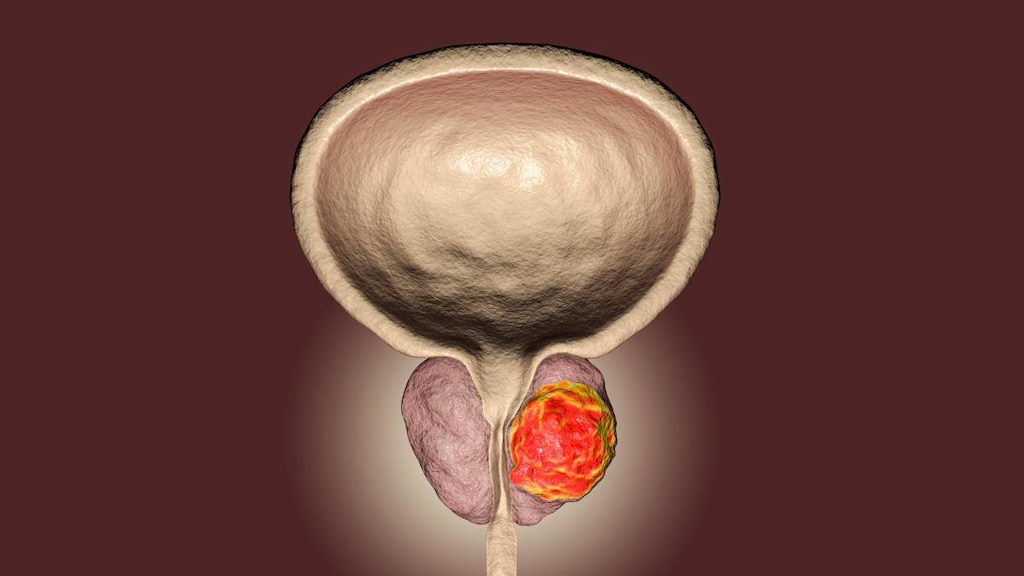
Prostate cancer is cancer that occurs in the prostate, which is a small, walnut-sized gland that is located just below the bladder in men and which surrounds the urethra (the tube that urine comes out of).
Prostate cancer is common, and many men have a slow-growing form of prostate cancer. Death, when it happens, is usually from other causes rather than cancer itself. However, some prostate cancers are aggressive and can quickly spread outside the confines of the prostate. These are associated with a lower rate of survival.
What causes prostate cancer?
Cancer is the uncontrollable growth of cells. It occurs when a mutation or abnormal change occurs that upsets how our cells multiply and divide. This allows the cell to keep dividing, out-of-control, instead of dying and being replaced by a new cell. Sometimes these out-of-control cells cluster together and form a lump called a tumor. Tumors can form in almost any area of the body.
Most prostate cancers develop from the glandular epithelial cells in the prostate - these are the cells that make prostate fluid, which is one of the main components of semen. Cancer that starts in the glandular cells is called an adenocarcinoma. Other types of cancer that can start in the prostate, such as small cell carcinomas, neuroendocrine tumors, and sarcomas, are rare.
Experts aren’t sure why some men develop prostate cancer and others don’t; however, they have identified a few risk factors that make some men more likely to develop the condition. These include:
- A family history of prostate cancer
- Age: The risk of prostate cancer increases with age especially after the age of 50. More than 80% of prostate cancers are diagnosed in men aged 65 or older
- Agent Orange exposure
- Diet and lifestyle. Excess red meat, fried foods, high-fat dairy products, high alcohol intake, and a lack of fruits and vegetables may also increase risk
- Geographical location. Prostate cancer is more common in North America and northern Europe. The incidence is also increasing among Asian men living in urbanized environments, such as Hong Kong, Singapore, and North American and European cities, particularly among those who do not do much physical activity or with a poor diet
- Hereditary breast and ovarian cancer (HBOC) syndrome. Men with HBOC have an increased risk of developing breast cancer and a more aggressive form of prostate cancer
- Race/ethnicity. African-American men have a higher risk of prostate cancer than white men. They are also more likely to develop prostate cancer at an earlier age and to have more aggressive tumors that grow quickly. Hispanic men have a lower risk of developing prostate cancer and dying from the disease than non-Hispanic Caucasian men
- Smoking
What are the symptoms of prostate cancer?
Many men with prostate cancer have no symptoms at all. If the cancer grows and presses on the urethra (the tube that carries urine out of your body) or spreads to the bladder it can cause:
- A weak urine stream or need to urinate more often
- Blood in the urine or semen
- Erection problems
- Lower back pain
- Pain during urination
How is prostate cancer diagnosed?
Prostate cancer may be suspected based on your symptoms or the results of a screening test.
Screening is when your doctor looks for cancer before you have any symptoms. This can help find cancer at an early stage when it may be easier to treat. Two of the most frequently used screening tests for prostate cancer include the digital rectal exam (DRE) and the prostate-specific antigen (PSA) test.
- A digital rectal exam (DRE) is an examination of the rectum where the doctor inserts a lubricated, gloved finger into the lower part of the rectum to feel for lumps or enlargement in the prostate gland
- A prostate-specific antigen (PSA) is a blood test that measures levels of PSA in your blood. However, PSA is reasonably nonspecific and high levels may be associated with prostate cancer, prostatitis (a non-cancerous condition), or an enlarged prostate gland. Very high levels of PSA (10 ng/mL and above) are associated with a 50% chance of prostate cancer
There is controversy over whether screening tests should be used at all. The US Preventive Services Task Force (USPSTF) recommends men aged 55 to 69 have a discussion with their doctor about the pros and cons of PSA screening to determine if it is an appropriate preventive test for them. For men aged 70 and older, the USPSTF does not recommend PSA screening.
The American Cancer Society, recommends early-detection screening starting at age 40 or 45 if men are at high risk, or age 50 in men at average risk.
In some cases, a prostate biopsy or an imaging test such as an ultrasound or magnetic resonance imaging (MRI) may also be used to rule out cancer.
How is prostate cancer treated?
Treatment for prostate cancer depends upon the stage of the prostate cancer and an understanding of the pros and cons of treatment.
Treatment options include:
- Watchful waiting. No active treatment is started. This may be appropriate for older men with other serious medical conditions
- Active watching. May involve regular PSA tests and prostate biopsies
- Radiation
- Brachytherapy. Small radioactive pellets are placed permanently into the prostate gland
- Surgery
- Anti-androgen drugs (hormone therapy)
- Chemotherapy