Boxed Warning
Serious cardiovascular risk:
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction (MI), and stroke, which can be fatal. This risk may occur early in the treatment and may increase with duration of use.
Celecoxib is contraindicated in the setting of coronary artery bypass graft (CABG) surgery.
Serious gastrointestinal risk:
NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events, including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at higher risk for serious GI events.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
CeleBREX: 50 mg, 100 mg, 200 mg, 400 mg
Generic: 50 mg, 100 mg, 200 mg, 400 mg
Pharmacology
Mechanism of Action
Inhibits prostaglandin synthesis by decreasing the activity of the enzyme, cyclooxygenase-2 (COX-2), which results in decreased formation of prostaglandin precursors; has antipyretic, analgesic, and anti-inflammatory properties. Celecoxib does not inhibit cyclooxygenase-1 (COX-1) at therapeutic concentrations.
Pharmacokinetics/Pharmacodynamics
Absorption
Prolonged due to low solubility
Distribution
Vd (apparent): Children and Adolescents ~7-16 years (steady-state): 8.3 ± 5.8 L/kg (Stempak 2002); Adults: ~400 L
Metabolism
Hepatic via CYP2C9; forms inactive metabolites (a primary alcohol, corresponding carboxylic acid, and its glucuronide conjugate)
Excretion
Feces (~57% as metabolites, <3% as unchanged drug); urine (27% as metabolites, <3% as unchanged drug); primary metabolites in feces and urine: Carboxylic acid metabolite (73% of dose); low amounts of glucuronide metabolite appear in urine
Time to Peak
Children: Median: 3 hours (range: 1-5.8 hours) (Stempak 2002); Adults: ~3 hours
Half-Life Elimination
Children and Adolescents ~7-16 years (steady-state): 6 ± 2.7 hours (range: 3-10 hours) (Stempak 2002); Adults: ~11 hours (fasted)
Protein Binding
~97% primarily to albumin; binds to alpha1-acid glycoprotein to a lesser extent
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC is approximately 40% lower in patients with a CrCl of 35 to 60 mL/minute.
Special Populations: Hepatic Function Impairment
AUC is increased approximately 40% in patients with mild impairment and 180% in patients with moderate impairment.
Special Populations: Elderly
Cmax is 40% higher and AUC is 50% higher.
Special Populations: Children
The AUC and Cmax following administration of a capsule contents sprinkled on applesauce were reported to be similar as administration of an intact capsule (Krishnaswami 2012).
Special Populations: Race
AUC is approximately 40% higher in black compared with white patients.
Use: Labeled Indications
Acute pain: Management of acute pain.
Ankylosing spondylitis: Relief of the signs/symptoms of ankylosing spondylitis.
Juvenile idiopathic arthritis: Relief of the signs/symptoms of juvenile idiopathic arthritis (JIA) in patients 2 years and older.
Osteoarthritis: Relief of the signs/symptoms of osteoarthritis.
Primary dysmenorrhea: Treatment of primary dysmenorrhea.
Rheumatoid arthritis: Relief of the signs/symptoms of rheumatoid arthritis.
Use: Off Label
Gout, acute flaresbyes
Data from a multinational, randomized, double-blind, controlled trial demonstrate efficacy of celecoxib for the treatment of acute gout flares Schumacher 2012. Clinical experience also supports the utility of celecoxib for this condition Becker 2018.
Based on the American College of Rheumatology guidelines for the management of acute gout flares, celecoxib is an effective and recommended treatment option for patients with GI contraindications or intolerance to nonselective NSAIDs.
Contraindications
Hypersensitivity to celecoxib, sulfonamides, aspirin, other NSAIDs, or any component of the formulation; patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs; use in the setting of CABG surgery.
Note: Although the FDA approved product labeling states this medication is contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See “Warnings/Precautions” for more detail.
Canadian labeling: Additional contraindications (not in US labeling): Pregnancy (third trimester); women who are breast-feeding; severe, uncontrolled heart failure; active gastrointestinal ulcer (gastric, duodenal, peptic); active gastrointestinal bleeding; inflammatory bowel disease; cerebrovascular bleeding; severe liver impairment or active hepatic disease; severe renal impairment (CrCl <30 mL/minute) or deteriorating renal disease; known hyperkalemia; use in patients <18 years of age
Dosage and Administration
Dosing: Adult
Note: Use the lowest effective dose for the shortest duration of time, consistent with individual patient treatment goals. Due to an increased risk of cardiovascular events, use should generally be avoided in patients with established cardiovascular disease or risk factors for cardiovascular disease. Use should also be avoided in those with heart failure (Chan 2018; Schmidt 2016).
Acute pain or primary dysmenorrhea: Oral: Initial dose: 400 mg, followed by an additional 200 mg if needed on day 1; maintenance dose: 200 mg twice daily as needed
Ankylosing spondylitis: Oral: 200 mg once daily or 100 mg twice daily; if no effect after 6 weeks, may increase to 400 mg/day. If no response following 6 weeks of treatment with 400 mg/day, consider discontinuation and alternative treatment.
Gout, acute flare (alternative agent) (off-label use): Oral: 200 mg twice daily; initiate within 24 to 48 hours of flare onset preferably; discontinue 2 to 3 days after resolution of clinical signs; usual duration: 5 to 7 days (ACR [Khanna 2012]; Becker 2018)
Osteoarthritis: Oral: 200 mg once daily or 100 mg twice daily
Rheumatoid arthritis: Oral: 100 to 200 mg twice daily
Dosing adjustment in poor CYP2C9 metabolizers (ie, CYP2C9*3/*3): Reduce initial dose by 50%; consider alternative treatment in patients with JIA who are poor CYP2C9 metabolizers.
Dosing: Geriatric
Initiate at the lowest recommended dose. The AUC in elderly patients (especially females and patients weighing <50 kg) may be increased by 50% compared with younger subjects.
Dosing: Pediatric
Juvenile idiopathic arthritis (JIA): Note: Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals.
Children ≥2 years and Adolescents:
≥10 kg to ≤25 kg: Oral: 50 mg twice daily
>25 kg: Oral: 100 mg twice daily
Dosing adjustment in poor metabolizers of CYP2C9 substrates: Use with caution in patients who are known or suspected poor metabolizers of cytochrome P450 isoenzyme 2C9 substrates.
Children ≥2 years and Adolescents: Consider alternate therapy in JIA patients who are poor metabolizers; experience in adult patients suggests dosing adjustment.
Administration
May be administered without regard to meals. Capsules may be swallowed whole or the entire contents emptied onto a teaspoon of cool or room temperature applesauce and administered immediately with water. The contents of the capsules sprinkled onto applesauce may be stored under refrigeration for up to 6 hours.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
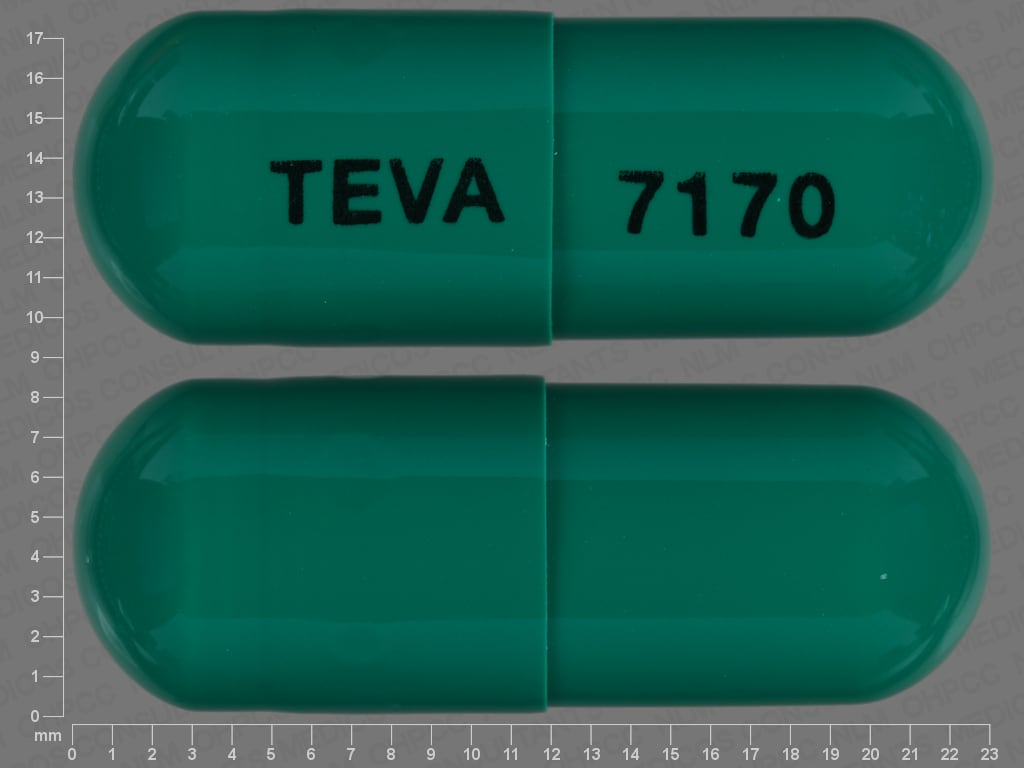
Celecoxib Images
Drug Interactions
5-Aminosalicylic Acid Derivatives: Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of 5-Aminosalicylic Acid Derivatives. Monitor therapy
Acemetacin: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of GI bleeding may be increased with this combination. Monitor therapy
Aliskiren: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Aliskiren. Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Aliskiren. Management: Monitor renal function periodically in patients receiving aliskiren and any nonsteroidal anti-inflammatory agent. Patients at elevated risk of renal dysfunction include those who are elderly, are volume depleted, or have pre-existing renal dysfunction. Monitor therapy
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Aminoglycosides: Nonsteroidal Anti-Inflammatory Agents may decrease the excretion of Aminoglycosides. Data only in premature infants. Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Angiotensin II Receptor Blockers: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Angiotensin II Receptor Blockers. The combination of these two agents may also significantly decrease glomerular filtration and renal function. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticoagulants: Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may enhance the anticoagulant effect of Anticoagulants. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Aspirin: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Management: Concurrent use of aspirin at doses beyond cardioprotective levels is not recommended. While concurrent use of low-dose aspirin with a COX-2 inhibitor is permissable, patients should be monitored closely for signs/symptoms of GI ulceration/bleeding. Consider therapy modification
Bemiparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin and nonsteroidal anti-inflammatory agents (NSAIDs) due to the increased risk of bleeding. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Beta-Blockers: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Nonsteroidal Anti-Inflammatory Agents. Consider therapy modification
Bisphosphonate Derivatives: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Both an increased risk of gastrointestinal ulceration and an increased risk of nephrotoxicity are of concern. Monitor therapy
Corticosteroids (Systemic): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Monitor therapy
CycloSPORINE (Systemic): Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of CycloSPORINE (Systemic). Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Management: Consider alternatives to nonsteroidal anti-inflammatory agents (NSAIDs). Monitor for evidence of nephrotoxicity, as well as increased serum cyclosporine concentrations and systemic effects (eg, hypertension) during concomitant therapy with NSAIDs. Consider therapy modification
CYP2C9 Inducers (Moderate): May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Deferasirox: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Desmopressin: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dexibuprofen: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Dexibuprofen. Avoid combination
Dexketoprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Digoxin: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Digoxin. Monitor therapy
Drospirenone: Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
Enoxaparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue nonsteroidal anti-inflammatory agents (NSAIDs) prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Eplerenone: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Eplerenone. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Eplerenone. Monitor therapy
Estrogen Derivatives: Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may enhance the thrombogenic effect of Estrogen Derivatives. Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Felbinac: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Floctafenine: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Haloperidol: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Haloperidol. Specifically including drowsiness and confusion. Monitor therapy
Heparin: Nonsteroidal Anti-Inflammatory Agents may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or nonsteroidal anti-inflammatory agents (NSAIDs) if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Bleeding may occur. Management: Concomitant treatment with these agents should generally be avoided. If used concomitantly, increased diligence in monitoring for adverse effects (eg, bleeding, bruising, altered mental status due to CNS bleeds) must be employed. Consider therapy modification
HydrALAZINE: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of HydrALAZINE. Monitor therapy
Ketorolac (Nasal): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Ketorolac (Systemic): May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Lithium: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Lithium. Consider therapy modification
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Loop Diuretics: Nonsteroidal Anti-Inflammatory Agents may diminish the diuretic effect of Loop Diuretics. Loop Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Monitor for evidence of kidney injury or decreased therapeutic effects of loop diuretics with concurrent use of an NSAID. Consider avoiding concurrent use in CHF or cirrhosis. Concomitant use of bumetanide with indomethacin is not recommended. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Macimorelin: Nonsteroidal Anti-Inflammatory Agents may diminish the diagnostic effect of Macimorelin. Avoid combination
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
MetFORMIN: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Methotrexate: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Methotrexate. Management: Alternative anti-inflammatory therapy should be considered whenever possible, especially if the patient is receiving higher, antineoplastic doses of methotrexate. Consider therapy modification
Mifamurtide: Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Mifamurtide. Avoid combination
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
Morniflumate: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Naftazone: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Avoid combination
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Avoid combination
Omacetaxine: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of nonsteroidal antiinflammatory drugs (NSAIDs) with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Pelubiprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
Phenylbutazone: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Potassium-Sparing Diuretics: Nonsteroidal Anti-Inflammatory Agents may diminish the antihypertensive effect of Potassium-Sparing Diuretics. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
PRALAtrexate: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of PRALAtrexate. More specifically, NSAIDS may decrease the renal excretion of pralatrexate. Management: Closely monitor for increased pralatrexate serum levels and/or toxicity if used concomitantly with an NSAID. Monitor for decreased pralatrexate serum levels with NSAID discontinuation. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Probenecid: May increase the serum concentration of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Prostaglandins (Ophthalmic): Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Prostaglandins (Ophthalmic). Nonsteroidal Anti-Inflammatory Agents may also enhance the therapeutic effects of Prostaglandins (Ophthalmic). Monitor therapy
Quinolones: Nonsteroidal Anti-Inflammatory Agents may enhance the neuroexcitatory and/or seizure-potentiating effect of Quinolones. Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Quinolones. Monitor therapy
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Phosphates: May enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with NSAIDs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. Consider therapy modification
Tacrolimus (Systemic): Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Tacrolimus (Systemic). Monitor therapy
Talniflumate: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Tenofovir Products: Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Tenofovir Products. Management: Seek alternatives to these combinations whenever possible. Avoid use of tenofovir with multiple NSAIDs or any NSAID given at a high dose. Consider therapy modification
Tenoxicam: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tolperisone: Nonsteroidal Anti-Inflammatory Agents may enhance the adverse/toxic effect of Tolperisone. Specifically, the risk of hypersensitivity reactions may be increased. Tolperisone may enhance the therapeutic effect of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Tricyclic Antidepressants (Tertiary Amine): May enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Monitor therapy
Triflusal: Nonsteroidal Anti-Inflammatory Agents may decrease the protein binding of Triflusal. Specifically, NSAIDs may decrease protein binding of the active Triflusal metabolite. Triflusal may decrease the protein binding of Nonsteroidal Anti-Inflammatory Agents. Monitor therapy
Vancomycin: Nonsteroidal Anti-Inflammatory Agents may increase the serum concentration of Vancomycin. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Zaltoprofen: May enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Avoid combination
Adverse Reactions
≥2%:
Cardiovascular: Peripheral edema (2%)
Gastrointestinal: Diarrhea (6%), dyspepsia (9%), abdominal pain (4%), flatulence (2%), gastroesophageal reflux disease, vomiting
Hepatic: Increased liver enzymes (<3x ULN: ≤6%)
Renal: Nephrolithiasis (3%)
Respiratory: Upper respiratory tract infection (8%), sinusitis (5%), pharyngitis (2%), rhinitis (2%), dyspnea
Miscellaneous: Accidental injury (3%)
Frequency not defined:
Dermatologic: Acute generalized exanthematous pustulosis, exfoliative dermatitis
Gastrointestinal: Gastrointestinal perforation, gastrointestinaI ulcer, GI inflammation, intestinal perforation
Hypersensitivity: Anaphylaxis
Immunologic: DRESS syndrome
Respiratory: Local alveolar osteitis (post oral surgery patients)
<2%, postmarketing, and/or case reports: Acute renal failure, ageusia, agranulocytosis, albuminuria, alopecia, anaphylactoid reaction, anemia, angina pectoris, angioedema, anorexia, anosmia, anxiety, aplastic anemia, arthralgia, aseptic meningitis, ataxia, bronchitis, bronchospasm, bronchospasm (aggravated), cellulitis, cerebrovascular accident, chest pain, cholelithiasis, colitis (with bleeding), constipation, contact dermatitis, coronary artery disease, cough, cyst, cyst (NOS), cystitis, deafness, decreased hemoglobin, deep vein thrombosis, depression, dermatitis, diaphoresis, diverticulitis, drowsiness, dysphagia, dysuria, ecchymoses, edema, epistaxis, eructation, erythema multiforme, erythematous rash, esophageal perforation, esophagitis, exacerbation of hypertension, facial edema, fatigue, fever, flu-like symptoms, gangrene of skin or other tissue, gastritis, gastroenteritis, gastroesophageal reflux disease, gastrointestinal hemorrhage, hematuria, hemorrhoids, hepatic failure, hepatic necrosis, hepatitis, hiatal hernia, hot flash, hypercholesterolemia, hyperglycemia, hypersensitivity exacerbation, hypersensitivity reaction, hypertonia, hypoesthesia, hypoglycemia, hypokalemia, hyponatremia, increased appetite, increased blood urea nitrogen, increased creatine phosphokinase, increased nonprotein nitrogen, increased serum alkaline phosphatase, interstitial nephritis, intestinal obstruction, intracranial hemorrhage, jaundice, laryngitis, leg cramps, leukopenia, maculopapular rash, melena, migraine, myalgia, myocardial infarction, nervousness, osteoarthritis, pain, palpitations, pancreatitis, pancytopenia, paresthesia, peripheral pain, pneumonia, pruritus, pulmonary embolism, skin changes, skin photosensitivity, Stevens-Johnson syndrome, stomatitis, syncope, synovitis, tachycardia, tendonitis, tenesmus, thrombocythemia, thrombocytopenia, thrombophlebitis, tinnitus, toxic epidermal necrolysis, urinary frequency, urticaria, vasculitis, ventricular fibrillation, vertigo, weight gain, xeroderma, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactoid reactions: Even in patients without prior exposure, anaphylactic reactions and angioedema may occur; patients with "aspirin triad" (bronchial asthma, aspirin intolerance, rhinitis) may be at increased risk. Contraindicated in patients who have experienced an anaphylactic reaction with nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin therapy.
- Cardiovascular events: [US Boxed Warning]: NSAIDs cause an increased risk of serious (and potentially fatal) adverse cardiovascular thrombotic events, including MI and stroke. Risk may occur early during treatment and may increase with duration of use. Relative risk appears to be similar in those with and without known cardiovascular disease or risk factors for cardiovascular disease; however, absolute incidence of cardiovascular events (which may occur early during treatment) was higher in patients with known cardiovascular disease or risk factors. New onset hypertension or exacerbation of hypertension may occur (NSAIDs may also impair response to ACE inhibitors, thiazide diuretics, or loop diuretics); may contribute to cardiovascular events; monitor blood pressure; use with caution in patients with hypertension. May cause sodium and fluid retention, use with caution in patients with edema. Avoid use in patients with heart failure (ACCF/AHA [Yancy 2013]). Avoid use in patients with recent MI unless benefits outweigh risk of cardiovascular thrombotic events. Long-term cardiovascular risk in children has not been evaluated. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of cardiovascular events; alternate therapies should be considered for patients at high risk.
- Gastrointestinal events: [US Boxed Warning]: NSAIDs cause an increased risk of serious gastrointestinal inflammation, ulceration, bleeding, and perforation (may be fatal); elderly patients and patients with history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events. These events may occur at any time during therapy and without warning. Avoid use in patients with active GI bleeding. Use caution with a history of GI ulcers, concurrent therapy known to increase the risk of GI bleeding (eg, aspirin, anticoagulants and/or corticosteroids, selective serotonin reuptake inhibitors), smoking, use of alcohol, or in elderly or debilitated patients. Use the lowest effective dose for the shortest duration of time, consistent with individual patient goals, to reduce risk of GI adverse events; alternate therapies should be considered for patients at high risk. When used concomitantly with aspirin, a substantial increase in the risk of gastrointestinal complications (eg, ulcer) occurs; concomitant gastroprotective therapy (eg, proton pump inhibitors) is recommended (Bhatt 2008).
- Hematologic effects: Anemia may occur; monitor hemoglobin or hematocrit in patients on long-term treatment. Celecoxib does not usually affect PT, PTT or platelet counts; does not inhibit platelet aggregation at approved doses.
- Skin reactions: NSAIDs may cause serious skin adverse events including exfoliative dermatitis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN); may occur without warning and in patients without prior known sulfa allergy; discontinue use at first sign of rash (or any other hypersensitivity).
- Sulfonamide ("sulfa") allergy: The FDA-approved product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
Disease-related concerns:
- Asthma: The manufacturer’s labeling states to not administer to patients with aspirin-sensitive asthma due to severe and potentially fatal bronchospasm that has been reported in such patients having received aspirin and the potential for cross reactivity with other NSAIDs. The manufacturer also states to use with caution in patients with other forms of asthma. However, in patients with known aspirin-exacerbated respiratory disease (AERD), the use of celecoxib initiated at a low dose with gradual titration in patients with stable, mild to moderate persistent asthma has been used without incident (Morales 2013).
- Bariatric surgery: Gastric ulceration: Avoid chronic use of oral nonselective NSAIDs after bariatric surgery; development of anastomotic ulcerations/perforations may occur (Bhangu 2014; Mechanick 2013). Short-term use of celecoxib or IV ketorolac are recommended as part of a multimodal pain management strategy for postoperative pain (Chou 2016; Horsley 2019; Thorell 2016).
- Coronary artery bypass graft surgery: [US Boxed Warning]: Celecoxib is contraindicated in the setting of coronary artery bypass graft surgery (CABG). Risk of MI and stroke may be increased with use following CABG surgery.
- Cytochrome P450 isoenzyme 2C9 deficiency: Use with caution in patients with known or suspected deficiency of cytochrome P450 isoenzyme 2C9; poor metabolizers may have higher plasma levels due to reduced metabolism; consider reduced initial doses. Alternate therapies should be considered in patients with JIA who are poor metabolizers of CYP2C9.
- Hepatic impairment: Use with caution in patients with moderate hepatic impairment; dosage adjustment recommended. Not recommended for patients with severe hepatic impairment. Transaminase elevations have been reported with use; closely monitor patients with any abnormal LFT. Rare (sometimes fatal), severe hepatic reactions (eg, fulminant hepatitis, hepatic necrosis, hepatic failure) have occurred with NSAID use; discontinue if signs or symptoms of liver disease develop, if systemic manifestations occur, or with persistent or worsening abnormal hepatic function tests.
- Renal impairment: NSAID use may compromise existing renal function. Dose-dependent decreases in prostaglandin synthesis may result from NSAID use, causing a reduction in renal blood flow which may cause renal decompensation (usually reversible). Patients with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics, ACE inhibitors, angiotensin II receptor blockers, and the elderly are at greater risk for renal toxicity. Rehydrate patient before starting therapy; monitor renal function closely. Avoid use in patients with advanced renal disease; discontinue use with persistent or worsening abnormal renal function tests. Long-term NSAID use may result in renal papillary necrosis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Use with caution in pediatric patients with systemic-onset juvenile idiopathic arthritis (JIA); serious adverse reactions, including disseminated intravascular coagulation, may occur.
Monitoring Parameters
CBC; hemoglobin/hematocrit (anemic patients); basic metabolic panel; occult blood loss and periodic liver function tests; monitor renal function (urine output, serum BUN and creatinine); monitor response (pain, range of motion, grip strength, mobility, ADL function), inflammation; blood pressure (baseline and during treatment); observe for weight gain, edema; observe for bleeding, bruising; evaluate gastrointestinal effects (abdominal pain, bleeding, dyspepsia)
JIA: Monitor for development of abnormal coagulation tests with systemic onset JIA
Pregnancy
Pregnancy Risk Factor
C (prior to 30 weeks' gestation)/D (≥30 weeks' gestation)
Pregnancy Considerations
Birth defects have been observed following in utero NSAID exposure in some studies, however data is conflicting (Bloor 2013). Nonteratogenic effects, including prenatal constriction of the ductus arteriosus, persistent pulmonary hypertension of the newborn, oligohydramnios, necrotizing enterocolitis, renal dysfunction or failure, and intracranial hemorrhage have been observed in the fetus/neonate following in utero NSAID exposure. In addition, nonclosure of the ductus arteriosus postnatally may occur and be resistant to medical management (Bermas 2014; Bloor 2013). Because NSAIDs may cause premature closure of the ductus arteriosus, product labeling for celecoxib specifically states use should be avoided starting at 30 weeks' gestation.
Use of NSAIDs can be considered for the treatment of mild rheumatoid arthritis flares in pregnant women, however use should be minimized or avoided early and late in pregnancy (Bermas 2014; Saavedra Salinas 2015). Some guidelines recommend avoiding use of selective Cox-2 inhibitors completely during pregnancy due to limited data (Flint 2016).
The chronic use of NSAIDs in women of reproductive age may be associated with infertility that is reversible upon discontinuation of the medication. Consider discontinuing use in women having difficulty conceiving or those undergoing investigation of fertility. The use of NSAIDs close to conception may be associated with an increased risk of miscarriage (Bermas 2014; Bloor 2013).
Patient Education
What is this drug used for?
- It is used to ease pain and swelling.
- It is used to treat arthritis.
- It is used to ease painful period (menstrual) cycles.
- It is used to treat ankylosing spondylitis.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal pain
- Heartburn
- Nausea
- Vomiting
- Constipation
- Diarrhea
- Passing gas
- Common cold symptoms
- Sore throat
- Stuffy nose
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Abdominal ulcers like severe abdominal or back pain; black, tarry, or bloody stools; vomiting blood or vomit that looks like coffee grounds; or weight gain or abnormal swelling.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, numbness or tingling feeling.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Severe headache
- Vision changes
- Severe dizziness
- Passing out
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Chest pain
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.