Boxed Warning
Concurrent drug therapy:
Serious and/or life-threatening peripheral ischemia has been associated with the coadministration of ergotamine/caffeine with potent CYP 3A4 inhibitors including protease inhibitors and macrolide antibiotics. Because CYP 3A4 inhibition elevates the serum levels of ergotamine/caffeine, the risk for vasospasm leading to cerebral ischemia and/or ischemia of the extremities is increased. Hence, concomitant use of these medications is contraindicated.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suppository, rectal:
Migergot: Ergotamine tartrate 2 mg and caffeine 100 mg (12s)
Tablet, oral:
Cafergot: Ergotamine tartrate 1 mg and caffeine 100 mg
Generic: Ergotamine tartrate 1 mg and caffeine 100 mg
Pharmacology
Mechanism of Action
Has partial agonist and/or antagonist activity against tryptaminergic, dopaminergic and alpha-adrenergic receptors depending upon their site; is a highly active uterine stimulant; it causes constriction of peripheral and cranial blood vessels and produces depression of central vasomotor centers
Pharmacokinetics/Pharmacodynamics
Absorption
Ergotamine: Oral, rectal: Erratic (Perrin, 1985)
Metabolism
Ergotamine: Extensively hepatic, including high first-pass metabolism (Perrin, 1985)
Excretion
Ergotamine: Feces (90%, primarily as metabolites) (Perrin, 1985)
Time to Peak
Serum: Ergotamine: 2 hours (Perrin, 1985)
Half-Life Elimination
2 to 2.5 hours (Perrin, 1985)
Use: Labeled Indications
Vascular headache: Prevention or treatment of vascular headaches, such as migraine, migraine variants, or so-called “histaminic cephalalgia”
Contraindications
Hypersensitivity to ergotamine, caffeine, or any component of the formulation; peripheral vascular disease; hepatic or renal impairment; coronary heart disease; hypertension; sepsis; concomitant use of ergot alkaloids with strong inhibitors of CYP3A4 (includes HIV and HCV protease inhibitors, cobicistat, azole antifungals, and some macrolide antibiotics); pregnancy
Dosage and Administration
Dosing: Adult
Vascular headache:
Oral: Note: Each tablet contains ergotamine 1 mg and caffeine 100 mg: Ergotamine 2 mg and caffeine 200 mg (2 tablets) at onset of attack; then ergotamine 1 mg and caffeine 100 mg (1 tablet) every 30 minutes as needed
Maximum dose: Ergotamine 6 mg and caffeine 600 mg (6 tablets) per attack; do not exceed ergotamine 10 mg and caffeine 1,000 mg (10 tablets) per week
Rectal: Ergotamine 2 mg and caffeine 100 mg (1 suppository) at first sign of an attack; follow with second dose after 1 hour, if needed
Maximum dose: Ergotamine 4 mg and caffeine 200 mg (2 suppositories) per attack; do not exceed ergotamine 10 mg and caffeine 500 mg (5 suppositories) per week
Dosing: Pediatric
Migraine: Limited data available; efficacy results variable: Note:Not for chronic daily administration. Not a preferred agent; use of ergotamine has largely been replaced by newer agents with improved efficacy and adverse effect profile.
Adolescents:
Oral: Tablets (ergotamine 1 mg/caffeine 100 mg per tablet): Initial dose: 1 or 2 tablets at onset of attack; then 1 tablet every 30 minutes as needed up to 4 additional doses; maximum dose per attack: 6 tablets (ergotamine 6 mg/caffeine 600 mg); maximum weekly dose: 10 tablets/week (ergotamine 10 mg/caffeine 1,000 mg). Note: Some experts have recommended lower maximum doses (maximum dose per attack: ergotamine 3 mg/attack; maximum weekly dose: ergotamine 5 mg/week) in patients <14 years (Géraud 2004; Krupp 1953; Nelson 1996; Singer 1994; Welborn 1997)
Rectal: Suppository (ergotamine 2 mg/caffeine 100 mg per suppository): Initial: 1/2 suppository (ergotamine 1 mg/caffeine 50 mg) at first sign of an attack; may repeat in 45 minutes if necessary. Maximum dose per attack: 1 suppository (ergotamine 2 mg/caffeine 100 mg)/attack; maximum dose per day: 2 suppositories (ergotamine 4 mg/caffeine 200 mg)/attack; maximum weekly dose: 4 suppositories (ergotamine 8 mg/caffeine 400 mg)/week (Singer 1994)
Administration
Oral: Administer with or without food.
Rectal: Suppository: Remove foil from rectal suppository and insert pointed end first. Avoid handling unwrapped suppository for too long.
Storage
Suppositories: Store refrigerated at 2°C to 8°C (36°F to 46°F) in sealed foil.
Tablet: Store at 20°C to 25°C (68°F to 77°F). Protect from light.
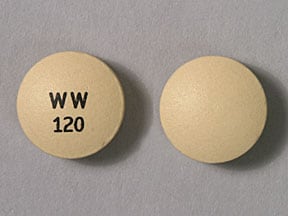
Ergotamine and Caffeine Images
Drug Interactions
Acebrophylline: May enhance the stimulatory effect of CNS Stimulants. Avoid combination
Adenosine: Caffeine and Caffeine Containing Products may diminish the therapeutic effect of Adenosine. Management: Monitor for decreased effect of adenosine if patient is receiving caffeine. Discontinue caffeine in advance of scheduled diagnostic use of adenosine whenever possible. Consider therapy modification
Alpha-/Beta-Agonists: Ergot Derivatives may enhance the hypertensive effect of Alpha-/Beta-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha-/Beta-Agonists. Avoid combination
Alpha1-Agonists: Ergot Derivatives may enhance the hypertensive effect of Alpha1-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha1-Agonists. Avoid combination
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Antihepaciviral Combination Products: May increase the serum concentration of Ergot Derivatives. Avoid combination
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Beta-Blockers: May enhance the vasoconstricting effect of Ergot Derivatives. Consider therapy modification
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Bromperidol: Caffeine and Caffeine Containing Products may decrease the absorption of Bromperidol. Monitor therapy
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Chloroprocaine: May enhance the hypertensive effect of Ergot Derivatives. Monitor therapy
Clarithromycin: May increase the serum concentration of Ergotamine. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Cobicistat: May increase the serum concentration of Ergotamine. Avoid combination
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Crizotinib: May increase the serum concentration of Ergotamine. Avoid combination
CYP1A2 Inducers (Moderate): May decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
CYP1A2 Inhibitors (Strong): May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Doxofylline: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Doxofylline. Avoid combination
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of Ergotamine. Avoid combination
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Esketamine: May enhance the hypertensive effect of CNS Stimulants. Monitor therapy
Formoterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Formoterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Formoterol. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Indacaterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Indacaterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Indacaterol. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Itraconazole: May increase the serum concentration of Ergotamine. Avoid combination
Ketoconazole (Systemic): May increase the serum concentration of Ergotamine. Avoid combination
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Letermovir: May increase the serum concentration of Ergot Derivatives. Avoid combination
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Lithium: Caffeine and Caffeine Containing Products may decrease the serum concentration of Lithium. Monitor therapy
Lorcaserin: May enhance the adverse/toxic effect of Ergot Derivatives. Specifically, use of these drugs together may increase the risk of developing valvular heart disease. Lorcaserin may enhance the serotonergic effect of Ergot Derivatives. This could result in serotonin syndrome. Avoid combination
Macrolide Antibiotics: May increase the serum concentration of Ergot Derivatives. Cabergoline and Clarithromycin may interact, see specific monograph for full details. Exceptions: Azithromycin (Systemic); Fidaxomicin; Spiramycin. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of Ergotamine. Management: Avoid ergotamine during and 2 weeks following mifepristone for treatment of hyperglycemia in Cushing's syndrome. The interaction magnitude could be lower with single doses used to terminate pregnancy, but neither effect has been studied clinically. Avoid combination
Nefazodone: Ergot Derivatives may enhance the serotonergic effect of Nefazodone. This could result in serotonin syndrome. Nefazodone may increase the serum concentration of Ergot Derivatives. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nitroglycerin: Ergot Derivatives may diminish the vasodilatory effect of Nitroglycerin. This is of particular concern in patients being treated for angina. Nitroglycerin may increase the serum concentration of Ergot Derivatives. Avoid combination
Norfloxacin: May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Olodaterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Olodaterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Olodaterol. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pipemidic Acid: May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Posaconazole: May increase the serum concentration of Ergotamine. Avoid combination
Protease Inhibitors: May increase the serum concentration of Ergot Derivatives. Avoid combination
Reboxetine: May enhance the hypertensive effect of Ergot Derivatives. Monitor therapy
Regadenoson: Caffeine and Caffeine Containing Products may diminish the vasodilatory effect of Regadenoson. Management: Avoiding using caffeine or other methylxanthine containing products (e.g., theophylline) for at least 12 hours prior to the administration of regadenoson. Consider therapy modification
Roxithromycin: May increase the serum concentration of Ergot Derivatives. Avoid combination
Serotonergic Agents (High Risk): Ergot Derivatives may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nefazodone. Monitor therapy
Serotonin 5-HT1D Receptor Agonists (Triptans): Ergot Derivatives may enhance the vasoconstricting effect of Serotonin 5-HT1D Receptor Agonists (Triptans). Serotonin 5-HT1D Receptor Agonists (Triptans) may enhance the vasoconstricting effect of Ergot Derivatives. Avoid combination
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Solriamfetol: CNS Stimulants may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Stiripentol: May increase the serum concentration of Caffeine and Caffeine Containing Products. Avoid combination
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tobacco (Smoked): May decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Voriconazole: May increase the serum concentration of Ergotamine. Avoid combination
Adverse Reactions
Frequency not defined.
Cardiovascular: Bradycardia, cold extremities, ECG changes, edema, hypertension, ischemia, tachycardia, valvular sclerosis, vasospasm
Central nervous system: Numbness, paresthesia, precordial pain, vertigo
Dermatologic: Gangrene of skin or other tissue, pruritus
Gastrointestinal: Anal fissure (with overuse of suppository), nausea, rectal ulcer (with overuse of suppository), vomiting
Genitourinary: Retroperitoneal fibrosis
Neuromuscular & skeletal: Myalgia, weakness
Respiratory: Cyanosis, pleuropulmonary fibrosis
Warnings/Precautions
Concerns related to adverse effects:
- Cardiac valvular fibrosis: Ergot alkaloids have been associated (rarely) with fibrotic valve thickening (eg, aortic, mitral, tricuspid); usually associated with long-term, chronic use.
- Cardiovascular effects: Vasospasm or vasoconstriction can occur, possibly resulting in cyanosis, decreased cerebral blood flow, bradycardia or tachycardia, asystole, and hypertension; sustained vasoconstriction may also lead to intermittent claudication, precordial distress, and pain. Do not use in any patient at risk or predisposed to vascular effects of ergot alkaloids.
- Ergotism: Ergot alkaloid use may result in ergotism (intense vasoconstriction) resulting in peripheral vascular ischemia and possible gangrene. Ergotism is usually associated with overdosage or prolonged chronic use; do not exceed dosing guidelines and avoid prolonged administration.
- Pleural/retroperitoneal fibrosis: Rare cases of pleural and/or retroperitoneal fibrosis have been reported with prolonged daily administration.
Concurrent drug therapy issues:
- CYP3A4 inhibitors: [U.S. Boxed Warning]: Ergot alkaloids are contraindicated with potent inhibitors of CYP3A4 (includes protease inhibitors and some macrolide antibiotics). Serum levels of ergotamines may be elevated, leading to increased risk of vasospasm leading to cerebral ischemia and/or ischemia of extremities. Serious and/or life-threatening peripheral ischemia has been associated with concomitant use.
- Drug-drug interactions: Additional potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Avoid use in the elderly due to the vasoconstrictive properties and cardiovascular adverse effects associated with ergot alkaloids.
Dosage form specific issues:
- Rectal suppositories: Solitary rectal or anal ulcers have occurred rarely when suppositories are used in higher than recommended doses or with continual use of recommended doses for prolonged periods of time. After discontinuation, spontaneous healing occurs within 4 to 8 weeks.
Other warnings/precautions:
- Appropriate use: Do not use for prolonged daily administration; serious adverse effects are associated with long-term continuous use. Use caution and remain within recommended dosage limits.
- Medication-overuse headache/Withdrawal: Discontinuation even after limited use may result in withdrawal symptoms (ie, rebound headache, nausea, vomiting).
Monitoring Parameters
BUN, serum creatinine, liver function tests at baseline, signs of peripheral ischemia (eg, vasospasm, digit coldness, and pallor), numbness, muscle pains, extremity weakness, chest pain, tachycardia or bradycardia, hypersensitivity reactions.
Pregnancy
Pregnancy Considerations
Ergotamine and caffeine both cross the placenta. Use is contraindicated in pregnant women. Refer to individual monographs for additional information.
Patient Education
What is this drug used for?
- It is used to treat migraine headaches.
Frequently reported side effects of this drug
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Chest pain
- Slow heartbeat
- Fast heartbeat
- Abnormal heartbeat
- Shortness of breath
- Swelling of arms or legs
- Excessive weight gain
- Swelling
- Severe dizziness
- Passing out
- Severe headache
- Vision changes
- Muscle weakness
- Muscle pain
- Change in color of hands or feet from pale to blue or red
- Sensation of cold in extremities
- Numbness, pain, or tingling in extremities
- Rectal sores
- Rectal pain
- Wounds on fingers or toes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.