Boxed Warning
Cigarette smoke and serious cardiovascular events:
Cigarette smoking increases the risk of serious cardiovascular events from combination oral contraceptives use. This risk increases with age, particularly in women over 35 years of age, and with the number of cigarettes smoked. For this reason, combination oral contraceptives should not be used by women who are over 35 years of age and smoke.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Kit, Oral:
FaLessa: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [contains brilliant blue fcf (fd&c blue #1), fd&c blue #2 (indigotine), fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake, soybean lecithin]
Tablet, Oral:
Afirmelle: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [contains fd&c blue #2 aluminum lake]
Altavera: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets]
Amethia: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains brilliant blue fcf (fd&c blue #1), corn starch]
Amethia Lo: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains corn starch, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Amethia Lo: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [DSC] [contains fd&c blue #1 aluminum lake]
Amethyst: Ethinyl estradiol 0.02 mg and levonorgestrel 0.09 mg [28 tablets]
Ashlyna: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Aubra: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets]
Aubra EQ: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [contains fd&c blue #2 aluminum lake]
Aviane: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets]
Ayuna: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets] [contains fd&c blue #2 aluminum lake, fd&c yellow #6 aluminum lake]
Balcoltra: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets] and ferrous bisglycinate 36.5 mg [7 tablets] [contains brilliant blue fcf (fd&c blue #1), fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 (sunset yellow), soybean lecithin]
Camrese: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Camrese Lo: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake, polysorbate 80]
Chateal: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets] [contains fd&c blue #1 aluminum lake]
Chateal EQ: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets] [contains fd&c blue #2 aluminum lake, fd&c yellow #6 aluminum lake]
Daysee: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #6 (sunset yellow)]
Delyla: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets]
Enpresse-28: Day 1-6: Ethinyl estradiol 0.03 mg and levonorgestrel 0.05 mg [6 tablets]; Day 7-11: Ethinyl estradiol 0.04 mg and levonorgestrel 0.075 mg [5 tablets]; Day 12-21: Ethinyl estradiol 0.03 mg and levonorgestrel 0.125 mg [10 tablets]; Day 22-28: 7 inactive tablets
Falmina: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [contains fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake, soybean lecithin]
Fayosim: Day 1-42: Ethinyl estradiol 0.02 mg and levonorgestrel 0.15 mg [42 tablets]; Day 43-63: Ethinyl estradiol 0.025 mg and levonorgestrel 0.15 mg [21 tablets]; Day 64-84: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets]; Day 85-91: Ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Introvale: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets and 7 inactive tablets]
Jaimiess: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets]
Jolessa: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets and 7 inactive tablets] [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Kurvelo: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets] [contains fd&c yellow #6 (sunset yellow)]
Larissia: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets]
Lessina: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [contains fd&c red #40 aluminum lake]
Levonest: Day 1-6: Ethinyl estradiol 0.03 mg and levonorgestrel 0.05 mg [6 tablets]; Day 7-11: Ethinyl estradiol 0.04 mg and levonorgestrel 0.075 mg [5 tablets]; Day 12-21: Ethinyl estradiol 0.03 mg and levonorgestrel 0.125 mg [10 tablets]; Day 22-28: 7 inactive tablets [contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake, soybean lecithin]
Levora 0.15/30 (28): Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets] [contains fd&c yellow #6 aluminum lake]
Lillow: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets]
LoJaimiess: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets]
LoSeasonique: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake, polysorbate 80]
Lutera: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets]
Marlissa: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets] [contains fd&c yellow #6 (sunset yellow)]
Myzilra: Day 1-6: Ethinyl estradiol 0.03 mg and levonorgestrel 0.05 mg [6 tablets]; Day 7-11: Ethinyl estradiol 0.04 mg and levonorgestrel 0.075 mg [5 tablets]; Day 12-21: Ethinyl estradiol 0.03 mg and levonorgestrel 0.125 mg [10 tablets]; Day 22-28: 7 inactive tablets [DSC] [contains fd&c blue #2 (indigotine), fd&c red #40, fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Orsythia: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [contains corn starch, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Orsythia: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [DSC] [contains fd&c blue #2 (indigotine), fd&c red #40 aluminum lake]
Portia-28: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets]
Quartette: Day 1-42: Ethinyl estradiol 0.02 mg and levonorgestrel 0.15 mg [42 tablets]; Day 43-63: Ethinyl estradiol 0.025 mg and levonorgestrel 0.15 mg [21 tablets]; Day 64-84: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets]; Day 85-91: Ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Quasense: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets and 7 inactive tablets] [DSC] [contains fd&c yellow #6 aluminum lake]
Rivelsa: Day 1-42: Ethinyl estradiol 0.02 mg and levonorgestrel 0.15 mg [42 tablets]; Day 43-63: Ethinyl estradiol 0.025 mg and levonorgestrel 0.15 mg [21 tablets]; Day 64-84: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets]; Day 85-91: Ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Seasonique: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Setlakin: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets and 7 inactive tablets] [contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake, soybean lecithin]
Simpesse: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets] [contains brilliant blue fcf (fd&c blue #1), corn starch]
Sronyx: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets]
Trivora (28): Day 1-6: Ethinyl estradiol 0.03 mg and levonorgestrel 0.05 mg [6 tablets]; Day 7-11: Ethinyl estradiol 0.04 mg and levonorgestrel 0.075 mg [5 tablets]; Day 12-21: Ethinyl estradiol 0.03 mg and levonorgestrel 0.125 mg [10 tablets]; Day 22-28: 7 inactive tablets [DSC]
Trivora (28): Day 1-6: Ethinyl estradiol 0.03 mg and levonorgestrel 0.05 mg [6 tablets]; Day 7-11: Ethinyl estradiol 0.04 mg and levonorgestrel 0.075 mg [5 tablets]; Day 12-21: Ethinyl estradiol 0.03 mg and levonorgestrel 0.125 mg [10 tablets]; Day 22-28: 7 inactive tablets [contains corn starch]
Vienva: Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets] [contains corn starch, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Generic: Day 1-42: Ethinyl estradiol 0.02 mg and levonorgestrel 0.15 mg [42 tablets]; Day 43-63: Ethinyl estradiol 0.025 mg and levonorgestrel 0.15 mg [21 tablets]; Day 64-84: Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets]; Day 85-91: Ethinyl estradiol 0.01 mg [7 tablets], Day 1-6: Ethinyl estradiol 0.03 mg and levonorgestrel 0.05 mg [6 tablets]; Day 7-11: Ethinyl estradiol 0.04 mg and levonorgestrel 0.075 mg [5 tablets]; Day 12-21: Ethinyl estradiol 0.03 mg and levonorgestrel 0.125 mg [10 tablets]; Day 22-28: 7 inactive tablets, Ethinyl estradiol 0.02 mg and levonorgestrel 0.09 mg [28 tablets], Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [21 tablets and 7 inactive tablets], Ethinyl estradiol 0.02 mg and levonorgestrel 0.1 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets], Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [21 tablets and 7 inactive tablets], Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets and 7 inactive tablets], Ethinyl estradiol 0.03 mg and levonorgestrel 0.15 mg [84 tablets]; ethinyl estradiol 0.01 mg [7 tablets]
Pharmacology
Mechanism of Action
Combination hormonal contraceptives inhibit ovulation via a negative feedback mechanism on the hypothalamus, which alters the normal pattern of gonadotropin secretion of a follicle-stimulating hormone (FSH) and luteinizing hormone by the anterior pituitary. The follicular phase FSH and midcycle surge of gonadotropins are inhibited. In addition, combination hormonal contraceptives produce alterations in the genital tract, including changes in the cervical mucus, rendering it unfavorable for sperm penetration even if ovulation occurs. Changes in the endometrium may also occur, producing an unfavorable environment for nidation. Combination hormonal contraceptive drugs may alter the tubal transport of the ova through the fallopian tubes. Progestational agents may also alter sperm fertility.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Ethinyl estradiol: 4.3 L/kg; Levonorgestrel: 1.8 L/kg
Metabolism
Ethinyl estradiol: Hepatic via CYP3A4; undergoes first-pass metabolism; forms metabolites
Levonorgestrel: Forms conjugated in unconjugated metabolites
Excretion
Ethinyl estradiol: Urine and feces
Levonorgestrel: Urine (40% to 68%, parent drug and metabolites); feces (16% to 48% as metabolites)
Half-Life Elimination
Ethinyl estradiol: 12-23 hours; Levonorgestrel: 22-49 hours
Protein Binding
Ethinyl estradiol: 95% to 97% to albumin
Levonorgestrel: 97% to 99% primarily to sex hormone binding globulin (SHBG), lesser amounts to albumin
Use: Labeled Indications
Contraception: Prevention of pregnancy.
Emergency contraception: Postcoital emergency contraception.
Limitations of use: Ethinyl estradiol in combination with levonorgestrel is effective and recommended as an alternative method for the management of emergency contraception when other methods are not available. The use of other methods is preferred due to increased side effects and decreased efficacy observed with this combination (AAP 2012; ACOG 2015)
Use: Off Label
Abnormal uterine bleedingyes
Based on the American College of Obstetricians and Gynecologists committee opinion on the management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women, ethinyl estradiol and levonorgestrel (among other oral contraceptive combinations) is effective and recommended for the management of abnormal uterine bleeding ACOG 2013.
Dysmenorrheayes
Based on the American College of Obstetricians and Gynecologists Practice Bulletin on Noncontraceptive Uses of Hormonal Contraceptives, ethinyl estradiol and levonorgestrel (among other oral contraceptive combinations) is effective and recommended for the management of dysmenorrhea ACOG 2010.
Hirsutismyes
Based on the Endocrine Society Clinical Practice Guideline for the Evaluation and Treatment of Hirsutism in Premenopausal Women, ethinyl estradiol and levonorgestrel is effective (among other oral estrogen-progestin contraceptive combinations) for the treatment of adult women with hirsutism; however, in women with hirsutism due to polycystic ovary syndrome (PCOS), the guidelines suggest that avoidance of levonorgestrel-containing products may be reasonable. This recommendation is based on the adverse effects of levonorgestrel on metabolic biomarkers and the common baseline metabolic abnormalities found in women with PCOS, although no specific outcomes data is available. In general, oral contraceptive therapy is recommended for initial therapy in most women of reproductive potential who are not seeking fertility Endocrine Society [Martin 2018].
Menstrual bleeding (menorrhagia)yes
Based on the American College of Obstetricians and Gynecologists Practice Bulletin on Noncontraceptive Uses of Hormonal Contraceptives, ethinyl estradiol and levonorgestrel (among other oral contraceptive combinations) is effective and recommended for the management of menstrual bleeding (menorrhagia) ACOG 2010.
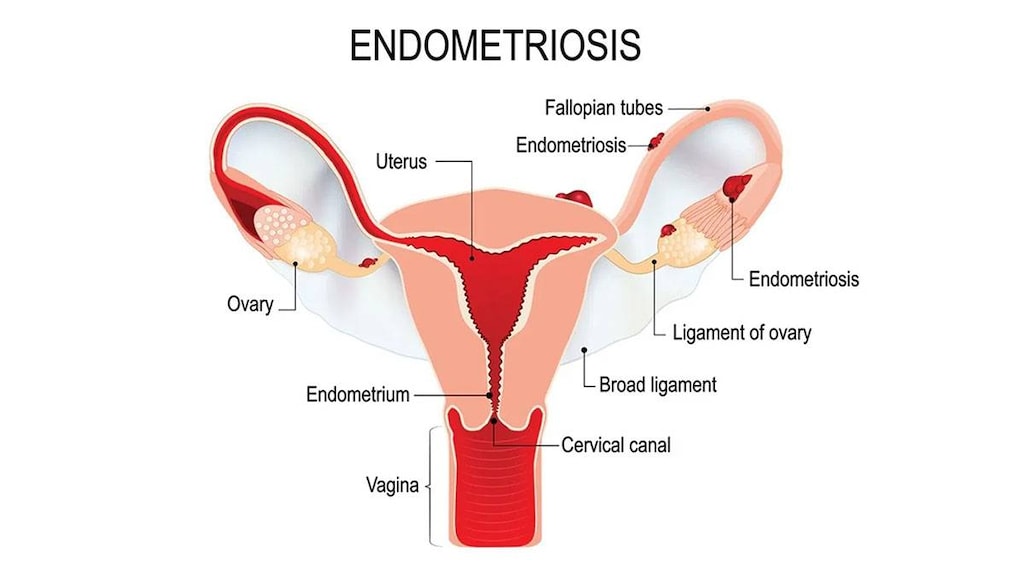
Pain associated with endometriosisyes
Based on the American College of Obstetricians and Gynecologists Practice Bulletin on Noncontraceptive Uses of Hormonal Contraceptives, ethinyl estradiol and levonorgestrel (among other oral contraceptive combinations) is effective and recommended for the management of pain associated with endometriosis ACOG 2010.
Polycystic ovary syndrome (PCOS) in women with menstrual irregularities and hirsutism/acneyes
Based on the Endocrine Society Clinical Practice Guideline for the Diagnosis and Treatment of Polycystic Ovary Syndrome, combined estrogen-progestin contraceptives are effective and recommended for the treatment of menstrual irregularities and hirsutism/acne in women with PCOS ES [Legro 2013]. However, the more recent Endocrine Society guidelines for the Evaluation and Treatment of Hirsutism in Premenopausal Women suggest that avoidance of levonorgestrel-containing products may be reasonable in women with hirsutism due to PCOS. This recommendation is based on the adverse effects of levonorgestrel on metabolic biomarkers and the common baseline metabolic abnormalities found in women with PCOS, although no specific outcomes data is available Endocrine Society [Martin 2018].
Contraindications
Breast cancer or other estrogen- or progestin-dependent neoplasms (current or a history of), hepatic tumors or disease, pregnancy; hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir
Use is also contraindicated in women at high risk of arterial or venous thrombotic diseases including: Cerebrovascular disease, coronary artery disease, diabetes mellitus with vascular disease, DVT or PE (current or history of), hypercoagulopathies (inherited or acquired), headaches with focal neurological symptoms, hypertension (uncontrolled), migraine headaches if >35 years of age, thrombogenic valvular or rhythm diseases of the heart (eg, subacute bacterial endocarditis with valvular disease or atrial fibrillation), women >35 years of age who smoke
Canadian labeling: Additional contraindication (not in the US labeling): Hypersensitivity to ethinyl estradiol, levonorgestrel, or any component of the formulation; ocular lesions due to ophthalmic vascular disease including partial or complete loss of vision or defect in visual fields; severe dyslipoproteinemia; persistent blood pressure ≥160 mm Hg systolic and ≥100 mm Hg diastolic; myocardial infarction (current or history of); prodromi of a thrombosis (eg, transient ischemic attack, angina pectoris; current or history of); major surgery associated with an increased risk of postoperative thromboembolism; prolonged immobilization; steroid-dependent jaundice, cholestatic jaundice, history of jaundice of pregnancy; pancreatitis if associated with severe hypertriglyceridemia (current or history of); women with hereditary or acquired predisposition for arterial or venous thrombosis, for example: Factor V Leiden mutation and activated protein C (APC-) resistance, antithrombin-III-deficiency, protein C deficiency, protein S deficiency, hyperhomocysteinemia (eg, due to MTHFR C677T, A1298 mutations), prothrombin mutation G20210A, and antiphospholipid-antibodies (anticardiolipin antibodies, lupus anticoagulant); coadministration with ombitasvir, paritaprevir, ritonavir (with or without dasabuvir or ribavirin); hereditary or acquired thrombophilias; abnormal liver function testing; undiagnosed abnormal vaginal bleeding
Documentation of allergenic cross-reactivity for estrogens and progestins is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Females:
Contraception: Oral: One tablet once daily. General dosing guidelines; refer to prescribing information for product specific information:
Schedule 1 (Sunday starter): Dose begins on first Sunday after onset of menstruation; if the menstrual period starts on Sunday, take first tablet that very same day. With a Sunday start, an additional method of contraception should be used until after the first 7 days of consecutive administration.
Schedule 2 (Day 1 starter): Dose starts on first day of menstrual cycle taking 1 tablet daily.
Missed or late doses (Curtis 2016a):
If one dose is late (<24 hours since dose should have been taken) or if one dose is missed (24 to <48 hours since dose should have been taken): Take dose as soon as possible. Continue remaining doses at the usual time (even if that means 2 doses on the same day).
If ≥2 consecutive doses are missed (≥48 hours since dose should have been taken): Take the most recently missed dose as soon as possible, discard any other missed doses. Continue remaining doses at the usual time (even if that means taking 2 doses on the same day); use back-up contraception until hormonal pills have been taken for 7 consecutive days. If doses were missed during the last week of hormonal (active) tablets (eg, days 15 to 21 of a 28-day pack), omit the hormone-free interval by finishing the current pack and starting a new pack. If unable to start a new pack immediately, back up contraception is needed until hormonal pills from a new pack have been taken for 7 consecutive days. Consider use of emergency contraception in some situations (refer to guidelines for details).
Also refer to prescribing information for product specific information.
Emergency Contraception: Oral (off label dosing): One dose followed by a second dose 12 hours later. Each dose should contain a minimum of ethinyl estradiol 100 mcg and levonorgestrel 0.5 mg. Although no longer available in a dedicated dosage form, available combination oral contraceptive pills can be used to achieve this dose. Treatment for emergency contraception should begin as soon as possible; however, treatment is still moderately effective if used within 5 days after unprotected or inadequately protected intercourse. Although routine use of antiemetics is not recommended, pretreatment may be considered for specific women (AAP 2012; ACOG 2015; Curtis 2016a).
Dosing: Pediatric
Females: Contraception or emergency contraception: Oral: Refer to adult dosing; not to be used prior to menarche.
Administration
Contraception: Administer at the same time each day.
Combined hormonal contraceptives may be initiated at any time during the menstrual cycle if it is reasonably sure the woman is not pregnant. Back-up contraception should be used for 7 days unless contraception is initiated within the first 5 days of menstrual bleeding or the woman abstains from sexual intercourse. Combined hormonal contraceptives may be started immediately following or within 7 days of a first or second trimester abortion; backup contraception is needed for 7 days unless contraception is started at the time of surgical abortion (Curtis 2016a).
Emergency contraception: If vomiting occurs within 3 hours, a second dose should be taken as soon as possible; consider use of an antiemetic (Curtis 2016a).
Storage
Store at 20°C to 25°C (68°F to 77°F).
Ethinyl Estradiol and Levonorgestrel Images
-

ethinyl estradiol/levonorgestrel ethinyl estradiol 0.02 mg / levonorgestrel 0.1 mg -

ethinyl estradiol/levonorgestrel ethinyl estradiol 0.01 mg -
ethinyl estradiol/levonorgestrel ethinyl estradiol 0.03 mg / levonorgestrel 0.15 mg -
ethinyl estradiol/levonorgestrel inert -

ethinyl estradiol/levonorgestrel 0.03 mg / 0.15 mg -

ethinyl estradiol/levonorgestrel inert
Drug Interactions
Ajmaline: Estrogen Derivatives may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Anastrozole: Estrogen Derivatives may diminish the therapeutic effect of Anastrozole. Avoid combination
Anthrax Immune Globulin (Human): Estrogen Derivatives may enhance the thrombogenic effect of Anthrax Immune Globulin (Human). Monitor therapy
Anticoagulants: Estrogen Derivatives may diminish the anticoagulant effect of Anticoagulants. More specifically, the potential prothrombotic effects of some estrogens and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of estrogens against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Consider therapy modification
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antihepaciviral Combination Products: Ethinyl Estradiol may enhance the hepatotoxic effect of Antihepaciviral Combination Products. Management: Use of ethinyl estradiol must be discontinued prior to use of this combination; ethinyl estradiol can be restarted 2 weeks after cessation of the antihepaciviral combination product. Avoid combination
Aprepitant: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use of a non-hormone-based contraceptive is recommended. Consider therapy modification
Armodafinil: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use alternative or concomitant methods of contraception in patients taking armodafinil and for one month after armodafinil discontinuation. Consider therapy modification
Artemether: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Consider the use of an alternative (i.e., non-hormonal) means of contraception in all women of childbearing potential who are using artemether. Consider therapy modification
Ascorbic Acid: May increase the serum concentration of Estrogen Derivatives. Monitor therapy
Asunaprevir: May decrease the serum concentration of Ethinyl Estradiol. Management: For patients using hormone-based contraception, a high-dose oral contraceptive containing at least 30 mcg of ethinyl estradiol combined with norethindrone acetate/norethindrone is recommended during treatment with asunaprevir. Consider therapy modification
Barbiturates: May diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a non-hormonal contraceptive is recommended. Consider therapy modification
Bexarotene (Systemic): May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Women of childbearing potential receiving bexarotene should use two reliable forms of contraception (including at least one nonhormonal form). Consider therapy modification
Bile Acid Sequestrants: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Administer estrogen-based oral contraceptives at least 1 to 4 hours prior to or 4 to 6 hours after administration of a bile acid sequestrant. Consider therapy modification
Bosentan: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use an alternative (i.e., non-hormonal) means of contraception for all women of childbearing potential who are using bosentan, and do not rely on hormonal contraceptives alone. Consider therapy modification
Brigatinib: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Females of childbearing potential should use an alternative, non-hormonal contraceptive during brigatinib therapy and for at least 4 months after the final brigatinib dose. Consider therapy modification
C1 inhibitors: Estrogen Derivatives may enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
CarBAMazepine: May diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a nonhormonal contraceptive is recommended. Consider therapy modification
Carfilzomib: May enhance the thrombogenic effect of Estrogen Derivatives (Contraceptive). Management: Consider alternative, non-hormonal methods of contraception in patients requiring therapy with carfilzomib. Consider therapy modification
Cenobamate: May decrease the serum concentration of Hormonal Contraceptives. Management: Women should use additional or alternative non-hormonal birth control while taking cenobamate. Consider therapy modification
Chenodiol: Estrogen Derivatives may diminish the therapeutic effect of Chenodiol. Management: Monitor clinical response to chenodiol closely when used together with any estrogen derivative. Monitor therapy
Cladribine: May diminish the therapeutic effect of Hormonal Contraceptives. Management: Women using systemically acting hormonal contraceptives should add a barrier method during cladribine dosing and for at least 4 weeks after the last dose in each treatment course. Consider therapy modification
CloBAZam: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Consider therapy modification
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Cobicistat: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Consider an alternative, nonhormone-based contraceptive in patients receiving cobicistat-containing products. Consider therapy modification
Colesevelam: May decrease the serum concentration of Ethinyl Estradiol. Management: Oral contraceptives containing ethinyl estradiol and norethindrone should be administered at least 4 hours before colesevelam. Consider therapy modification
Corticosteroids (Systemic): Estrogen Derivatives may increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Cosyntropin: Estrogen Derivatives may diminish the diagnostic effect of Cosyntropin. Management: Discontinue estrogen containing drugs 4 to 6 weeks prior to cosyntropin (ACTH) testing. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Estrogen Derivatives. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Estrogen Derivatives. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Females of reproductive potential should use an alternative, highly effective, non-hormonal means of contraception during and at least 2 weeks (dabrafenib alone) or 4 months (dabrafenib + trametinib) after discontinuation of dabrafenib treatment. Consider therapy modification
Dantrolene: Estrogen Derivatives may enhance the hepatotoxic effect of Dantrolene. Monitor therapy
Dasabuvir: Ethinyl Estradiol may enhance the hepatotoxic effect of Dasabuvir. Avoid combination
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dehydroepiandrosterone: May enhance the adverse/toxic effect of Estrogen Derivatives. Avoid combination
Elagolix: Estrogen Derivatives (Contraceptive) may diminish the therapeutic effect of Elagolix. Management: Use an alternative, non-hormonal contraceptive during treatment with elagolix and for at least 1 week following discontinuation of elagolix treatment. Consider therapy modification
Elexacaftor, Tezacaftor, and Ivacaftor: Hormonal Contraceptives may enhance the adverse/toxic effect of Elexacaftor, Tezacaftor, and Ivacaftor. Specifically, the risk for rash may be increased. Monitor therapy
Elvitegravir: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Consider the use of an alternative, non-hormone-based contraceptive, in patients who are being treated with elvitegravir-containing products. Consider therapy modification
Encorafenib: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Eslicarbazepine: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Alternative non-hormonal means of birth control should be considered for women of child-bearing potential. Consider therapy modification
Exemestane: Estrogen Derivatives may diminish the therapeutic effect of Exemestane. Avoid combination
Exenatide: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Administer oral contraceptives at least one hour prior to exenatide. Consider therapy modification
Felbamate: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a nonhormonal contraceptive is recommended. Consider therapy modification
Flibanserin: Estrogen Derivatives (Contraceptive) may increase the serum concentration of Flibanserin. Monitor therapy
Fosaprepitant: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). The active metabolite aprepitant is likely responsible for this effect. Management: Alternative or additional methods of contraception should be used both during treatment with fosaprepitant or aprepitant and for at least one month following the last fosaprepitant/aprepitant dose. Consider therapy modification
Fosphenytoin: May diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of an alternative, nonhormonal means of contraception is recommended. Consider therapy modification
Glecaprevir and Pibrentasvir: Ethinyl Estradiol may enhance the adverse/toxic effect of Glecaprevir and Pibrentasvir. Specifically, the risk for ALT elevation may be increased with this combination. Avoid combination
Griseofulvin: May increase the metabolism of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use an alternative, nonhormonal form of contraception, or use an alternative to griseofulvin. Consider therapy modification
Guanethidine: Estrogen Derivatives (Contraceptive) may diminish the therapeutic effect of Guanethidine. Monitor therapy
Hemin: Estrogen Derivatives may diminish the therapeutic effect of Hemin. Avoid combination
Herbs (Estrogenic Properties): May enhance the adverse/toxic effect of Estrogen Derivatives. Monitor therapy
Hyaluronidase: Estrogen Derivatives may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving estrogens (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Immune Globulin: Estrogen Derivatives may enhance the thrombogenic effect of Immune Globulin. Monitor therapy
Indium 111 Capromab Pendetide: Estrogen Derivatives may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Ivosidenib: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Consider alternative methods of contraception (ie, non-hormonal) in patients receiving ivosidenib. Consider therapy modification
Ixazomib: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). More specifically, use of ixazomib with dexamethasone may decrease the serum concentrations of estrogen derivative contraceptives. Management: Patients of childbearing potential should use a nonhormonal barrier contraceptive during and 90 days following ixazomib treatment. Consider therapy modification
LamoTRIgine: Estrogen Derivatives (Contraceptive) may decrease the serum concentration of LamoTRIgine. Management: Most patients taking estrogen-containing contraceptives will require lamotrigine dose increases up to 2-fold over the recommended target lamotrigine dose. Increase lamotrigine doses by 50 to 100 mg/day every week based on clinical response. Consider therapy modification
Lenalidomide: Estrogen Derivatives may enhance the thrombogenic effect of Lenalidomide. Monitor therapy
Lesinurad: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use of an additional, nonhormonal contraceptive is recommended in patients being treated with lesinurad who desire effective contraception. Consider therapy modification
Lixisenatide: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Administer oral contraceptives 1 hour before or at least 11 hours after administration of lixisenatide. Consider therapy modification
Lomitapide: Ethinyl Estradiol may increase the serum concentration of Lomitapide. Management: Patients on lomitapide 5 mg/day may continue that dose. Patients taking lomitapide 10 mg/day or more should decrease the lomitapide dose by half. The lomitapide dose may then be titrated up to a max adult dose of 40 mg/day. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of Hormonal Contraceptives. Management: Do not rely on hormone-based contraceptives with concurrent use of lumacaftor/ivacaftor; an alternative, non-hormonal, method of contraception should be used if this combination is required. Consider therapy modification
Metreleptin: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Metreleptin may increase the serum concentration of Estrogen Derivatives (Contraceptive). Monitor therapy
MiFEPRIStone: May diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). MiFEPRIStone may increase the serum concentration of Estrogen Derivatives (Contraceptive). Management: Women of childbearing potential should use an effective, nonhormonal means of contraception during and 4 weeks following mifepristone treatment. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Mivacurium: Estrogen Derivatives may increase the serum concentration of Mivacurium. Monitor therapy
Modafinil: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use alternative or concomitant methods of contraception in patients taking modafinil and for one month after modafinil discontinuation. Consider therapy modification
Mycophenolate: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Average AUC values were unchanged, but there was evidence of substantial patient-to-patient variability in response to this combination. Management: Women of childbearing potential who are receiving mycophenolate mofetil should consider using an alternative and/or additional form of contraception. Consider therapy modification
Nafcillin: May increase the metabolism of Estrogen Derivatives (Contraceptive). Management: Use of an alternative, nonhormonal form of contraception during nafcillin therapy is recommended. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): May enhance the thrombogenic effect of Estrogen Derivatives. Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Ospemifene: Estrogen Derivatives may enhance the adverse/toxic effect of Ospemifene. Estrogen Derivatives may diminish the therapeutic effect of Ospemifene. Avoid combination
OXcarbazepine: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Phenytoin: May diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of an alternative, nonhormonal means of contraception is recommended. Consider therapy modification
Pitolisant: May decrease the serum concentration of Hormonal Contraceptives. Management: Patients using hormonal contraception should be advised to use an alternative non-hormonal contraceptive method during treatment with pitolisant and for at least 21 days after discontinuation of pitolisant treatment. Consider therapy modification
Pomalidomide: May enhance the thrombogenic effect of Estrogen Derivatives. Management: Canadian pomalidomide labeling recommends caution with use of hormone replacement therapy and states that hormonal contraceptives are not recommended. US pomalidomide labeling does not contain these specific recommendations. Consider therapy modification
Proguanil: Ethinyl Estradiol may diminish the therapeutic effect of Proguanil. Monitor therapy
Protease Inhibitors: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use oral contraceptives containing at least 35mcg ethinyl estradiol with atazanavir/ritonavir, or no more than 30mcg in patients receiving atazanavir alone. Use of an alternative, non-hormonal contraceptive is recommended with other protease inhibitors. Exceptions: Indinavir. Consider therapy modification
Rifamycin Derivatives: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
ROPINIRole: Estrogen Derivatives may increase the serum concentration of ROPINIRole. Monitor therapy
Rufinamide: May decrease the serum concentration of Ethinyl Estradiol. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selegiline: Estrogen Derivatives (Contraceptive) may increase the serum concentration of Selegiline. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
St John's Wort: May diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Consider an alternative to St John's wort if possible. If this combination is used, an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Succinylcholine: Estrogen Derivatives may increase the serum concentration of Succinylcholine. Monitor therapy
Sugammadex: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Patients receiving any hormonal contraceptive (oral or non-oral) should use an additional, nonhormonal contraceptive method during and for 7 days following sugammadex treatment. Consider therapy modification
Tazemetostat: May decrease the serum concentration of Hormonal Contraceptives. Management: Women of reproductive potential should use a non-hormonal contraceptive method during treatment with tazemetostat and for 6 months after. Men with female partners should use contraception during treatment and for 3 months after. Consider therapy modification
Tetrahydrocannabinol and Cannabidiol: May decrease the serum concentration of Hormonal Contraceptives. Management: Women using hormonal contraceptives should consider adding a barrier contraceptive due to the potential for tetrahydrocannabinol and cannabidiol to decrease concentrations and effectiveness of hormonal contraceptives. Consider therapy modification
Thalidomide: Estrogen Derivatives (Contraceptive) may enhance the thrombogenic effect of Thalidomide. Monitor therapy
Thalidomide: Estrogen Derivatives may enhance the thrombogenic effect of Thalidomide. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Thyroid Products: Estrogen Derivatives may diminish the therapeutic effect of Thyroid Products. Monitor therapy
Tipranavir: Estrogen Derivatives may enhance the dermatologic adverse effect of Tipranavir. The combination of tipranavir/ritonavir and ethinyl estradiol/norethindrone was associated with a high incidence of skin rash. Tipranavir may decrease the serum concentration of Estrogen Derivatives. Management: Women using hormonal contraceptives should consider alternative, non-hormonal forms of contraception. Consider therapy modification
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tobacco (Smoked): May enhance the adverse/toxic effect of Estrogen Derivatives (Contraceptive). Specifically, the risk of serious cardiovascular events (eg, stroke, venous thromboembolism, myocardial infarction) may be increased. Management: Avoid cigarette smoking in patients who use estrogen containing contraceptives whenever possible. If combined, monitor for signs and symptoms of serious cardiovascular events (eg, stroke, venous thromboembolism, myocardial infarction). Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Topiramate: May decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Risk appears greatest for higher topiramate doses (200 mg/day or greater). Some have recommended using at least 50 mcg/day of ethinyl estradiol, but the effectiveness of this is unclear. Consider a nonhormonal form of contraception. Consider therapy modification
Tranexamic Acid: Estrogen Derivatives (Contraceptive) may enhance the thrombogenic effect of Tranexamic Acid. Avoid combination
Triazolam: Hormonal Contraceptives may increase the serum concentration of Triazolam. Monitor therapy
Ursodiol: Estrogen Derivatives may diminish the therapeutic effect of Ursodiol. Monitor therapy
Valproate Products: Estrogen Derivatives (Contraceptive) may decrease the serum concentration of Valproate Products. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Estrogen Derivatives (Contraceptive) may diminish the anticoagulant effect of Vitamin K Antagonists. In contrast, enhanced anticoagulant effects have also been noted with some products. Consider therapy modification
Voriconazole: May decrease the metabolism of Estrogen Derivatives (Contraceptive). Estrogen Derivatives (Contraceptive) may increase the serum concentration of Voriconazole. Monitor therapy
Adverse Reactions
Frequency not defined. Reactions listed are based on reports for other agents in this same pharmacologic class (oral contraceptives) and may not be specifically reported for ethinyl estradiol/levonorgestrel.
Increased risk or evidence of association with use:
Cardiovascular: Arterial thromboembolism, cerebral thrombosis, hypertension, local thrombophlebitis, mesenteric thrombosis, myocardial infarction, pulmonary embolism, retinal thrombosis, venous thrombosis (with or without embolism)
Central nervous system: Cerebral hemorrhage
Gastrointestinal: Gallbladder disease
Hepatic: Hepatic adenoma, hepatic neoplasm (benign)
Adverse reactions considered drug related:
Cardiovascular: Edema, worsening of varicose veins
Central nervous system: Depression, exacerbation of tics, migraine, mood changes
Dermatologic: Allergic skin rash, chloasma
Endocrine & metabolic: Amenorrhea, breast changes (breast hypertrophy, breast secretion, breast tenderness, mastalgia), carbohydrate intolerance, decreased lactation (with use immediately postpartum), decreased serum folate level, exacerbation of porphyria, fluid retention, menstrual disease (menstrual flow changes), weight changes
Gastrointestinal: Abdominal cramps, abdominal pain, bloating, change in appetite, nausea, vomiting
Genitourinary: Breakthrough bleeding, cervical ectropion, cervical erosion, change in cervical secretions, endocervical hyperplasia, infertility (temporary), spotting, vulvovaginal candidiasis, vaginitis
Hematologic & oncologic: Uterine fibroid enlargement
Hepatic: Cholestatic jaundice, hepatic focal nodular hyperplasia
Hypersensitivity: Anaphylaxis/Anaphylactoid reaction (including angioedema, circulatory shock, respiratory collapse, urticaria)
Neuromuscular & skeletal: Exacerbation of systemic lupus erythematosus
Ophthalmic: Change in corneal curvature (steepening), contact lens intolerance
Respiratory: Rhinitis
Adverse reactions in which association is not confirmed or denied:
Cardiovascular: Budd-Chiari syndrome
Central nervous system: Dizziness, headache, nervousness
Dermatologic: Acne vulgaris, erythema multiforme, erythema nodosum, loss of scalp hair
Endocrine & metabolic: Change in libido, hirsutism, premenstrual syndrome
Gastrointestinal: Colitis, pancreatitis
Genitourinary: Abnormal Pap smear, cystitis-like syndrome, dysmenorrhea
Hematologic & oncologic: Hemolytic-uremic syndrome, hemorrhagic eruption
Ophthalmic: Cataract, optic neuritis (with or without partial or complete loss of vision)
Otic: Auditory disturbance
Renal: Renal insufficiency
Warnings/Precautions
Concerns related to adverse effects:
- Breast cancer: In women at risk for breast cancer due to family history or susceptibility genes (BRCA1, BRCA2), the use of combination hormonal contraceptives has not been shown to modify the risk for breast cancer. However, breast cancer is a hormonal sensitive tumor and the prognosis for women with a current or recent history of breast cancer may be worse with combination hormonal contraceptive use (Curtis 2016b). Use is contraindicated in women with (or history of) breast cancer.
- Cervical cancer: The use of combination hormonal contraceptives has been associated with a slight increased risk of cervical cancer; however, studies are not consistent and may be related to additional risk factors (Gierisch 2013). Theoretically, use may affect prognosis of existing disease. Women awaiting treatment for cervical cancer may use combination hormonal contraceptives (Curtis 2016b).
- Chloasma: Combination hormonal contraceptives, as well as sun exposure and pregnancy, are triggers for chloasma. Women with a susceptibility to chloasma or additional risk factors should avoid exposure to sun or ultraviolet radiation during therapy (Handel 2014).
- Cholestasis: Risk of cholestasis may be increased with previous cholestatic jaundice of pregnancy or jaundice with prior oral contraceptive use.
- Lipid effects: Combination hormonal contraceptives may adversely affect lipid levels, including serum triglycerides. Women with hypertriglyceridemia or a family history of hypertriglyceridemia may be at increased risk of pancreatitis when using combination hormonal contraceptives. Consider alternative contraception for women with uncontrolled dyslipidemia.
- Retinal vascular thrombosis: Discontinue if unexplained loss of vision, proptosis, diplopia, papilledema, or retinal vascular lesions occur and immediately evaluate for retinal vein thrombosis.
- Thromboembolic disorders: Discontinue use of combination hormonal contraceptives if an arterial or venous thrombotic event occurs. Oral contraceptives may increase the risk of venous thromboembolism (risk is greatest during first year of use and less than the risk associated with pregnancy); some studies suggest this risk may be higher in preparations with third- or fourth-generation progestins and/or high dose ethinyl estradiol. Women with inherited thrombophilias (eg, protein C or S deficiency, factor V Leiden mutation, prothrombin mutation, antithrombin deficiency) may have increased risk of venous thromboembolism. Age >35 years, hypertension, obesity, and tobacco use also increase the risk of thrombotic events in women taking combination hormonal contraceptives (ASRM 2017; Curtis 2016b; DeSancho 2010; van Vlijmen 2011). Combination hormonal contraceptives may also increase the risk of arterial thrombosis (eg, MI, stroke) and should not be used in women with a history of stroke or ischemic heart disease (Curtis 2016b). Use of combination hormonal contraceptives is contraindicated in women with a high risk of arterial or venous thrombotic disease.
- Vaginal bleeding: Breakthrough or intracyclic bleeding and spotting may occur, especially during the first 3 months of therapy. In addition, occasional missed periods may occur. Presentation of irregular, unresolving vaginal bleeding warrants further evaluation to rule out malignancy or pregnancy. Amenorrhea or oligomenorrhea may occur after discontinuing combination hormonal contraceptives, especially when such a condition was preexistent.
Disease-related concerns:
- Bariatric surgery:
- Altered absorption: Consider nonoral contraceptive options in patients who had specific bariatric procedures (Roux-en-Y, biliopancreatic diversion); malabsorptive procedures can potentially decrease absorption of oral contraceptives (Kominiarek 2017; Mechanick 2013; Schlatter 2017). It is difficult to recommend against the use of oral contraceptives in restrictive procedures (sleeve gastrectomy, gastric banding) as the evidence is limited (Merki-Feld 2015).
- Venous thromboembolism risk: Consider discontinuation of estrogen-containing medications 30 days prior to bariatric surgery to reduce risk of venous thromboembolism; however, practice may vary based upon institutional protocols (Mechanick 2013).
- Cardiovascular disease: Use with caution in patients with risk factors for coronary artery disease (eg, hypertension, low HDL, high LDL, high triglycerides, older age, diabetes, women who smoke); use of combination hormonal contraceptives may increase the risk of cardiovascular disease (Curtis 2016b). Use of combination hormonal contraceptives may be contraindicated in women at high risk of arterial or venous thrombotic diseases
- Depression: Use with caution in patients with a high risk of depression; discontinue if serious depression recurs.
- Diabetes: May impair glucose tolerance; use caution in women with diabetes. In general, use of combination oral contraceptives has limited effects on daily insulin needs and no long term effects on diabetes control in women with nonvascular disease. However, use in women with concomitant nephropathy, neuropathy, retinopathy, other vascular disease, or diabetes >20 years duration should be evaluated for contraceptive use based on the severity of the condition (Curtis 2016b). Use is contraindicated in women with diabetes mellitus and vascular disease.
- Endometrial or ovarian cancer: The risk of endometrial or ovarian cancer is decreased in women using combination hormonal contraceptives (Curtis 2016b; Walker 2015). Oral contraceptives may be used to reduce the risk of ovarian cancer including those women with BRCA1 and BRCA2 mutations (Walker 2015). Women awaiting treatment for endometrial or ovarian cancer may use combination hormonal contraceptives (Curtis 2016b).
- Gallbladder disease: Combination hormonal contraceptives may cause a small increased risk of gallbladder disease or may worsen existing gallbladder disease (Curtis 2016b).
- Hepatic adenomas or carcinomas: Use of combination hormonal contraceptives is associated with hepatic adenomas (rare); rupture may cause fatal intra-abdominal hemorrhage. Long-term use may be associated with an increased risk of hepatocellular carcinoma (rare). Use is contraindicated with preexisting hepatic tumors.
- Hepatic impairment: Combination hormonal contraceptives may be poorly metabolized in women with hepatic impairment. Discontinue if jaundice develops during therapy or if liver function becomes abnormal. Use is contraindicated with preexisting hepatic disease. Use of combination hormonal contraceptives may be considered in women with mild (compensated) cirrhosis but should not be used in women with severe (decompensated) cirrhosis (Curtis 2016b).
- Hepatitis: Initiation of combination hormonal contraceptives is not recommended in women with acute viral hepatitis or during a flare. Continuation of use in women with chronic hepatitis has not been shown to increase the rate or severity of cirrhotic fibrosis or hepatocellular carcinoma. Continuation of use in women who are carriers has not been shown to trigger liver failure or severe hepatic dysfunction (Curtis 2016b).
- Hereditary angioedema: Estrogens may induce or exacerbate symptoms in women with hereditary angioedema (Geng 2013; Zuraw 2013).
- Hypertension: The risk of hypertension may be increased with age, dose, and duration of use. Combination hormonal contraceptives should not be used in women with hypertension and vascular disease, or persistent blood pressure values ≥160 mm Hg systolic or ≥100 mm Hg diastolic. The risks of use may not outweigh the benefits of treatment in women with less severe hypertension (140 to 159 mm Hg systolic or 90 to 99 mm Hg diastolic) or those with hypertension that is adequately controlled (Curtis 2016a). Other risk factors for cardiovascular disease (eg, older age, smoking, diabetes) should be considered when prescribing contraceptives (Curtis 2016b). The manufacturer contraindicates use in women with uncontrolled hypertension and recommends monitoring women with well-controlled hypertension; discontinue therapy if blood pressure rises significantly.
- Migraine: Evaluate new, recurrent, severe or persistent headaches. Use of combination hormonal contraceptives may be considered in women who have migraines without aura (including menstrual migraines) (Curtis 2016b). Use in women with headaches with focal neurological symptoms, or migraine headaches with or without aura if >35 years is contraindicated.
- Solid organ transplant: Although data is limited, serious medical complications have been reported in women with complicated organ transplants (eg, graft failure, rejection, cardiac allograft vasculopathy); use of combination hormonal contraceptives is not recommended in women with complicated organ transplants (Curtis 2016b).
- Systemic lupus erythematosus (SLE): Women with SLE are at an increased risk for heart disease, stroke, and VTE. Combination hormonal contraceptives should not be used in women with SLE who have positive (or unknown) antiphospholipid antibodies, due to an increased risk of arterial and venous thrombosis (Curtis 2016b).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Thyroid replacement therapy: Estrogens may increase thyroid-binding globulin (TBG) levels leading to increased circulating total thyroid hormone levels. Women on thyroid replacement therapy may require higher doses of thyroid hormone while receiving estrogens.
Special populations:
- Obese: Available evidence suggests efficacy of combination hormonal contraceptives may be decreased in women with a BMI ≥30 kg/m2; however, reductions in effectiveness are considered minimal and information is conflicting. The risk of VTE may be increased in obese women using combination hormonal contraceptives. In general, the benefits of combination hormonal contraceptives may outweigh the risks in obese women who otherwise are eligible for this method (Curtis 2016b).
- Pediatric: Not for use prior to menarche.
- Postmenopausal women: Use is not indicated in postmenopausal women.
- Smokers: [US Boxed Warning]: Cigarette smoking increases the risk of serious cardiovascular events from combination oral contraceptives use. This risk increases with age, particularly in women >35 years of age, and with the number of cigarettes smoked. For this reason, combination oral contraceptives should not be used by women who are over 35 years and smoke. Use is contraindicated in patients >35 years of age who smoke.
- Surgical patients: Whenever possible, should be discontinued at least 4 weeks prior to and for 2 weeks following elective surgery associated with an increased risk of thromboembolism or during periods of prolonged immobilization.
Dosage form specific issues:
- Tartrazine: Some products may contain tartrazine, which may cause allergic reactions in certain individuals.
Other warnings/precautions:
- Extended cycle regimen: Contraceptives with an extended cycle regimen provide more hormonal exposure per year than conventional monthly contraceptives.
- HIV infection protection: Combination hormonal contraceptives do not protect against HIV infection or other sexually transmitted diseases (Curtis 2016a; Curtis 2016b).
- Laboratory changes: The use of estrogens and/or progestins may change the results of some laboratory tests (eg, coagulation factors, lipids, glucose tolerance, binding proteins).
Monitoring Parameters
Contraception:
Assessment of pregnancy status (prior to therapy); blood pressure (prior to therapy and yearly); weight (optional; BMI at baseline may be helpful to monitor changes during therapy); assess potential health status changes at routine visits (Curtis 2016a).
If all doses have not been taken on schedule and one menstrual period is missed, the possibility of pregnancy should be considered. If two consecutive menstrual periods are missed, assess pregnancy status before a new dosing cycle is started.
Monitor patient for vision changes; blood pressure; signs and symptoms of thromboembolic disorders; signs or symptoms of depression; glycemic control in patients with diabetes; lipid profiles in patients being treated for hyperlipidemias. Adequate diagnostic measures, including endometrial sampling, if indicated, should be performed to rule out malignancy in all cases of undiagnosed abnormal vaginal bleeding.
Emergency contraception: Evaluate for pregnancy, spontaneous abortion or ectopic pregnancy if menses is delayed for ≥1 week following emergency contraception, or if lower abdominal pain or persistent irregular bleeding develops (ACOG 2015).
Pregnancy
Pregnancy Risk Factor
X
Pregnancy Considerations
Use is contraindicated in pregnant women. Combination hormonal contraceptives are used to prevent pregnancy; treatment should be discontinued if pregnancy occurs. In general, the use of combination hormonal contraceptives, when inadvertently used early in pregnancy, have not been associated adverse fetal or maternal effects (Curtis 2016b).
Some manufacturers recommend waiting at least 4 to 6 weeks postpartum before starting this combination. Due to the increased risk of venous thromboembolism (VTE) postpartum, combination hormonal contraceptives should not be started in any woman <21 days following delivery. The risk decreases to baseline by postpartum day 42. Use of combination hormonal contraceptives in women between 21 and 42 days after delivery should take into consideration the individual woman's risk factors for VTE (eg, age ≥35 years, previous VTE, thrombophilia, immobility, preeclampsia, transfusion at delivery, cesarean delivery, peripartum cardiomyopathy, BMI ≥30 kg/m2, postpartum hemorrhage, smoking) (Curtis 2016b).
When used for emergency contraception, a barrier contraceptive is recommended immediately following use. Any regular (nonemergency) contraceptive method can be started immediately after combined estrogen/progestin emergency contraception; however, a barrier method (or abstinence from sexual intercourse) is also needed for 7 days (ACOG 2015; Curtis 2016a).
Patient Education
What is this drug used for?
- It is used to prevent pregnancy.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Lack of appetite
- Increased hunger
- Weight gain
- Weight loss
- Abdominal cramps
- Bloating
- Menstrual irregularities
- Tender breasts
- Enlarged breasts
- Dark patches on face
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Gallstones like pain in the upper right abdominal area, right shoulder area, or between the shoulder blades; yellow skin; or fever with chills.
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood.
- Mood changes
- Edema
- Severe dizziness
- Passing out
- Severe headache
- Depression
- Lump in breast
- Breast pain
- Breast soreness
- Nipple discharge
- Vaginal pain, itching, and discharge
- Abnormal or persistent vaginal bleeding
- Blindness
- Vision changes
- Vision loss
- Bulging eyes
- Contact lens discomfort
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.