Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
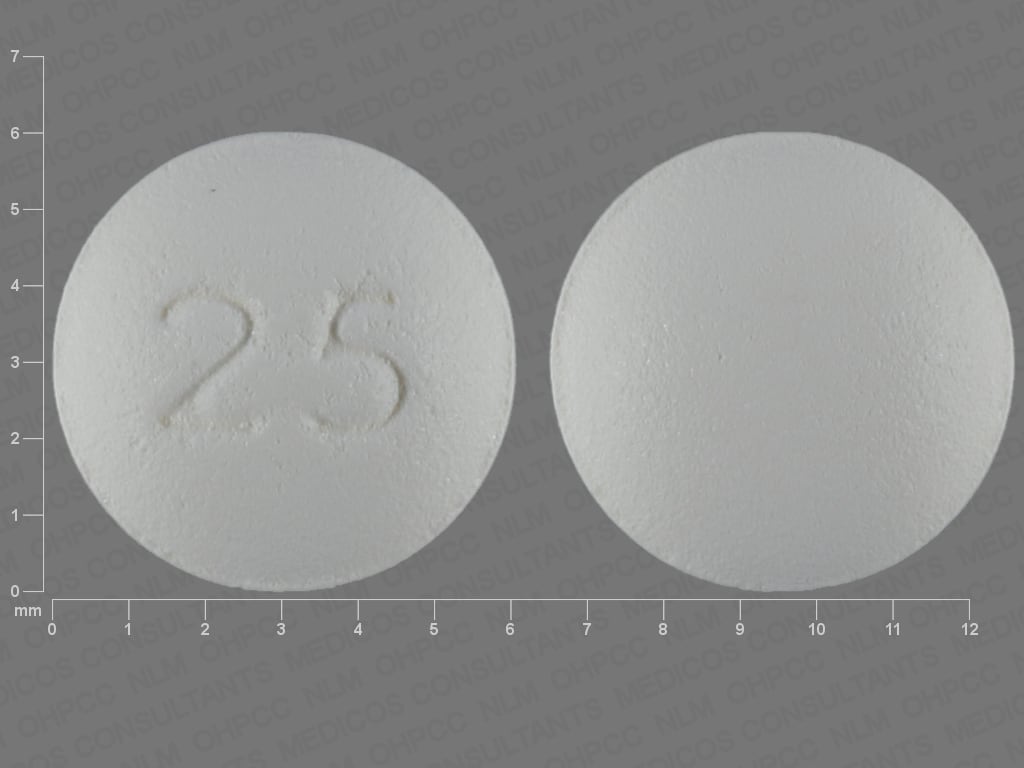
Tablet, Oral:
Aromasin: 25 mg
Generic: 25 mg
Pharmacology
Mechanism of Action
Exemestane is an irreversible, steroidal aromatase inactivator. It is structurally related to androstenedione, and is converted to an intermediate that irreversibly blocks the active site of the aromatase enzyme, leading to inactivation ("suicide inhibition") and thus preventing conversion of androgens to estrogens in peripheral tissues. Significantly lowers circulating estrogens in postmenopausal breast cancers where growth is estrogen-dependent.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and moderate (~42%) following oral administration; AUC and Cmax increased by 59% and 39%, respectively, following a high-fat breakfast (compared to fasted state)
Distribution
Extensive into tissues
Metabolism
Extensively hepatic; oxidation (CYP3A4) of methylene group, reduction of 17-keto group with formation of many secondary metabolites; metabolites are inactive
Excretion
Urine (<1% as unchanged drug, 39% to 45% as metabolites); feces (36% to 48%)
Time to Peak
Women with breast cancer: 1.2 hours
Half-Life Elimination
~24 hours
Protein Binding
90%, primarily to albumin and α1-acid glycoprotein
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC is approximately 3 times higher in those with moderate or severe renal insufficiency compared to patients with normal renal function.
Special Populations: Hepatic Function Impairment
AUC increased approximately 3 times in those with moderate or severe hepatic insufficiency compared to patients with normal hepatic function.
Use: Labeled Indications
Breast cancer: Treatment of advanced breast cancer in postmenopausal women whose disease has progressed following tamoxifen therapy; adjuvant treatment of postmenopausal women with estrogen receptor-positive early breast cancer following 2 to 3 years of tamoxifen (for a total of 5 consecutive years of adjuvant therapy).
Use: Off Label
First-line adjuvant treatment of estrogen receptor-positive early breast cancer in postmenopausal womenyesa
Data from a phase III, multicenter, multinational, randomized, open-label trial supports the use of exemestane in the treatment of this condition van de Veld 2011.
Based on the American Society of Clinical Oncology Clinical Practice Guidelines for Adjuvant Endocrine Therapy for Women with Hormone Receptor-Positive Breast Cancer, exemestane is effective and recommended as adjuvant treatment for early breast cancer.
Risk reduction for invasive breast cancer in postmenopausal womenyesa
Data from a randomized, placebo-controlled, double-blind trial supports the use of exemestane in this setting Goss 2011.
Based on the American Society of Clinical Oncology Clinical Practice Guidelines on the Use of Pharmacologic Interventions for Breast Cancer Risk, exemestane (as an alternative to tamoxifen and/or raloxifene) is effective and recommended to reduce the risk of invasive breast cancer (ie, ER-positive breast cancer) in post-menopausal women.
Contraindications
Known hypersensitivity to exemestane or any component of the formulation
Dosage and Administration
Dosing: Adult
Breast cancer, advanced: Postmenopausal females: Oral: 25 mg once daily; continue until tumor progression
Breast cancer, early (adjuvant treatment): Postmenopausal females: Oral: 25 mg once daily (following 2 to 3 years of tamoxifen therapy) for a total duration of 5 years of endocrine therapy (in the absence of recurrence or contralateral breast cancer).
Duration of therapy: American Society of Clinical Oncology (ASCO) guidelines for Adjuvant Endocrine Therapy of Hormone Receptor-Positive Breast Cancer (Focused Update) recommend a maximum duration of 5 years of aromatase inhibitor (AI) therapy for postmenopausal women; AIs may be combined with tamoxifen for a total duration of up to 10 years of endocrine therapy. Refer to the guidelines for specific recommendations based on menopausal status and tolerability (Burstein 2014). In a phase III study with another AI (letrozole), treatment with an additional 5 years of AI therapy (for a total of 10 years of aromatase inhibitor therapy) demonstrated a significantly improved rate of disease-free survival and a decreased risk of disease recurrence and contralateral breast cancer (when compared to placebo), although overall survival was not significantly different between groups and bone-related adverse events occurred more frequently with letrozole versus placebo (Goss 2016).
Breast cancer, early (first-line adjuvant treatment; off-label use): Postmenopausal females: Oral: 25 mg once daily for 5 years (Burstein 2010; van de Velde 2011).
Duration of therapy: ASCO guidelines for Adjuvant Endocrine Therapy of Hormone Receptor-Positive Breast Cancer (Focused Update) recommend a maximum duration of 5 years of aromatase inhibitor (AI) therapy for postmenopausal women; AIs may be combined with tamoxifen for a total duration of up to 10 years of endocrine therapy. Refer to the guidelines for specific recommendations based on menopausal status and tolerability (Burstein 2014). In a phase III study with another AI (letrozole), treatment with an additional 5 years of AI therapy (for a total of 10 years of aromatase inhibitor therapy) demonstrated a significantly improved rate of disease-free survival and a decreased risk of disease recurrence and contralateral breast cancer (when compared to placebo), although overall survival was not significantly different between groups and bone-related adverse events occurred more frequently with letrozole versus placebo (Goss 2016).
Breast cancer, risk reduction (off-label use): Postmenopausal females ≥35 years: Oral: 25 mg once daily for 5 years (Goss 2011; Visvanathan 2013)
Dosage adjustment with strong CYP3A4 inducers: 50 mg once daily when used with potent inducers (eg, rifampin, phenytoin)
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer after a meal.
Dietary Considerations
Patients on aromatase inhibitor therapy should receive vitamin D and calcium supplements.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
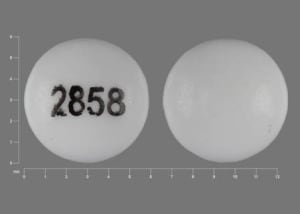
Exemestane Images
Drug Interactions
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Exemestane. Management: Exemestane U.S. product labeling recommends using an increased dose (50 mg/day) in patients receiving concurrent strong CYP3A4 inducers. The Canadian product labeling does not recommend a dose adjustment with concurrent use of strong CYP3A4 inducers. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Estrogen Derivatives: May diminish the therapeutic effect of Exemestane. Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Levomethadone: Aromatase Inhibitors may increase the serum concentration of Levomethadone. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Methadone: Aromatase Inhibitors may increase the serum concentration of Methadone. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
St John's Wort: May decrease the serum concentration of Exemestane. Management: Exemestane US product labeling recommends using an increased dose (50 mg/day) in patients receiving St Johns Wort or strong CYP3A4 inducers. The Canadian product labeling does not recommend a dose adjustment with this combination. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
Frequency not always defined. *Incidence not specifically defined, but reported in the range of 1% to 10%.
Cardiovascular: Hypertension (5% to 15%), edema (6% to 7%), ischemic heart disease (2%; angina pectoris, myocardial infarction), chest pain*
Central nervous system: Fatigue (8% to 22%), insomnia (11% to 14%), pain (13%), headache (7% to 13%), depression (6% to 13%), dizziness (8% to 10%), anxiety (4% to 10%), paresthesia (3%), carpal tunnel syndrome (2%), confusion,* hypoesthesia*
Dermatological: Hyperhidrosis (4% to 18%), alopecia (15%), dermatitis (8%), pruritus,* skin rash*
Endocrine & metabolic: Hot flash (13% to 33%), weight gain (8%), increased follicle-stimulating hormone, increased luteinizing hormone, increased sex hormone binding globulin (with daily doses of ≥2.5 mg; dose-dependent)
Gastrointestinal: Nausea (9% to 18%), abdominal pain (6% to 11%), diarrhea (4% to 10%), vomiting (7%), anorexia (6%), constipation (5%), increased appetite (3%), dyspepsia*
Genitourinary: Urinary tract infection (2% to 5%)
Hematologic & oncologic: Lymphedema*
Hepatic: Increased serum alkaline phosphatase (14% to 15%), increased serum bilirubin (5% to 7%)
Infection: Infection*
Neuromuscular & skeletal: Arthralgia (15% to 29%), back pain (9%), limb pain (9%), myalgia (6%), osteoarthritis (6%), weakness (6%), osteoporosis (5%), pathological fracture (4%), muscle cramps (2%)
Ophthalmic: Visual disturbance (5%)
Renal: Increased serum creatinine (6%)
Respiratory: Dyspnea (10%), cough (6%), flu-like symptoms (6%), bronchitis,* pharyngitis,* rhinitis,* sinusitis,* upper respiratory tract infection*
Miscellaneous: Fever (5%)
<1%, postmarketing, and/or case reports: Abnormal bone growth (osteochondrosis), acute generalized exanthematous pustulosis, cardiac failure, cholestatic hepatitis, endometrial hyperplasia, endometrial polyps, gastric ulcer, hepatitis, hypersensitivity reaction, increased gamma-glutamyl transferase, increased serum transaminases, neuropathy, tenosynovitis (fingers), thromboembolism, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Decreased bone mineral density: Due to decreased circulating estrogen levels, exemestane is associated with a reduction in bone mineral density over time. Decreases (from baseline) in lumbar spine and femoral neck density have been observed (when compared to tamoxifen or placebo in studies where concomitant use of bisphosphonates, calcium and vitamin D were not allowed). Assess bone mineral density at baseline in patients with, or at risk for osteoporosis; monitor during exemestane therapy and initiate osteoporosis treatment if indicated.
- Lymphopenia: Grade 3 or 4 lymphopenia has been observed with exemestane, although most patients had preexisting lower grade lymphopenia; some patients improved or recovered while continuing exemestane. Lymphopenia did not result in a significant increase in viral infections, and no opportunistic infections were observed.
- Lab parameters: Elevations of AST, ALT, alkaline phosphatase, and gamma glutamyl transferase >5 times ULN have been observed (rarely) in patients with advanced breast cancer; may be attributable to underlying liver and/or bone metastases. In patients with early breast cancer, elevations of bilirubin, alkaline phosphatase, and serum creatinine were more common with exemestane treatment than with tamoxifen or placebo.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information. Dose adjustment recommended with concomitant strong CYP3A4 inducers.
- Estrogen-containing drugs: Exemestane should not be administered concurrently with estrogen-containing drugs.
Other warnings/precautions:
- Appropriate use: Exemestane is not indicated for use in premenopausal women.
- Vitamin D deficiency: Due to high prevalence of vitamin D deficiency in women with breast cancer, assess 25-hydroxy vitamin D levels at baseline and supplement accordingly.
Monitoring Parameters
25-hydroxy vitamin D levels (at baseline); bone mineral density
Pregnancy
Pregnancy Considerations
Exemestane is not indicated for use in premenopausal women. Based on the mechanism of action and on animal data, exemestane is expected to cause fetal harm if administered to a pregnant woman. Women of reproductive potential should use effective contraception during treatment and for 1 month after the final dose. Pregnancy testing is recommended (for females of reproductive potential) within 7 days prior to therapy initiation.
Patient Education
What is this drug used for?
- It is used to treat breast cancer in women after change of life.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hot flashes
- Abdominal pain
- Nausea
- Vomiting
- Constipation
- Increased hunger
- Muscle pain
- Joint pain
- Hair loss
- Loss of strength and energy
- Trouble sleeping
- Sweating a lot
- Back pain
- Diarrhea
- Anxiety
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Edema
- Chest pain
- Bone pain
- Vision changes
- Depression
- Severe headache
- Severe dizziness
- Passing out
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.