Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Androxy: 10 mg [DSC] [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Pharmacology
Mechanism of Action
Synthetic derivative of testosterone; responsible for the normal growth and development of male sex hormones, male sex organs, and maintenance of secondary sex characteristics; large doses suppress endogenous testosterone release
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Metabolism
Hepatic; enterohepatic recirculation
Excretion
Urine (90%); feces (6%)
Half-Life Elimination
10 hours (range: 10-100 minutes)
Protein Binding
98%
Use: Labeled Indications
Breast cancer, metastatic (females): Salvage treatment of inoperable metastatic breast cancer in postmenopausal females
Delayed puberty (males): Replacement therapy in the treatment of delayed male puberty
Hypogonadism (males): Treatment of male hypogonadism (primary or hypogonadotropic)
Contraindications
Males with carcinoma of the breast or the prostate (known or suspected); women who are or may become pregnant
Dosage and Administration
Dosing: Adult
Note: Androxy has been discontinued in the US for more than 1 year.
Breast cancer, metastatic (females): Oral: Manufacturer labeling: 10 to 40 mg daily in divided doses for ≥3 months
Delayed puberty (males): Oral: 2.5 to 20 mg daily for 4 to 6 months
Hypogonadism, primary or hypogonadotropic (males): Oral: 5 to 20 mg daily
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Androxy has been discontinued in the US for more than 1 year.
Note: Dosage and duration of therapy depend upon age, sex, diagnosis, patient’s response to therapy, and appearance of adverse effects.
Delayed puberty: Adolescent Males: Typically not recommended for use before 14 years of age (Palmert 2012): Oral: Usual range: 2.5 mg to 10 mg daily, dose may be administered once daily or divided; reported range: 2.5 to 20 mg; most experts recommend a daily a dose of 2.5 mg for 6 to 60 months dependent upon clinical response (Melmed 2011; Strickland 1993); with testosterone therapy, response may be evaluated every 3 to 6 months and dose titrated as appropriate (Palmert 2012)
Male hypogonadism: Children ≥12 years and Adolescents (Han 2010; Young 2012): Oral: 2.5 to 20 mg daily; dose may be administered once daily or in divided doses for 4 to 6 months; some experts suggest beginning testosterone therapy with low doses and titrating gradually to prevent rapid over-virilization (Young 2012)
Dosing adjustment for toxicity: Children ≥12 years and Adolescents:
Edema: All patients: If therapy is discontinued due to edema, may reinitiate (if indicated) at a reduced dosage.
Hypogonadism: In adult males, the following have been suggested: Hematocrit (HCT) >50%: Use is not recommended; if HCT >54% during therapy, discontinue until HCT falls to a safe level, assess for hypoxia and sleep apnea; if reinitiating therapy, reduce the dose (Bhasin 2010)
Dosing: Adjustment for Toxicity
Edema: If therapy is discontinued due to edema, may reinitiate (if indicated) at a reduced dosage
Hypercalcemia during therapy for metastatic breast cancer (females): Discontinue use
Hypogonadism (males) (off-label): Hematocrit (HCT) >50%: Use is not recommended; if HCT >54% during therapy, discontinue until HCT falls to a safe level, assess for hypoxia and sleep apnea; if reinitiating therapy, reduce the dose (Bhasin 2010)
Administration
Males: May be administered in single or divided doses. Females: Administer in divided doses.
Storage
Store between 15°C to 30°C (59°F to 86°F); protect from light.
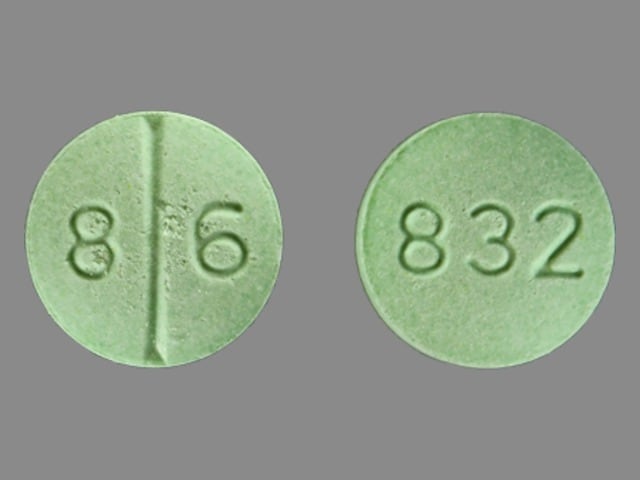
Fluoxymesterone Images
Drug Interactions
Ajmaline: Androgens may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Blood Glucose Lowering Agents: Androgens may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
C1 inhibitors: Androgens may enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
Corticosteroids (Systemic): May enhance the fluid-retaining effect of Androgens. Monitor therapy
CycloSPORINE (Systemic): Androgens may enhance the hepatotoxic effect of CycloSPORINE (Systemic). Androgens may increase the serum concentration of CycloSPORINE (Systemic). Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Androgens may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Test Interactions
Decreased levels of thyroxine-binding globulin; decreased total T4 serum levels; increased resin uptake of T3 and T4
Adverse Reactions
Frequency not defined.
Cardiovascular: Edema
Central nervous system: Anxiety, depression, headache, paresthesia
Dermatologic: Acne vulgaris, androgenetic alopecia
Endocrine & metabolic: Change in libido (decreased libido or increased libido), electrolyte disturbance (calcium, chloride, inorganic phosphate, potassium, and sodium retention), fluid retention, gynecomastia (males), hirsutism, hypercholesterolemia, menstrual disease (females; including amenorrhea)
Gastrointestinal: Gastrointestinal irritation, nausea, vomiting
Genitourinary: Benign prostatic hypertrophy (males), oligospermia (males; at higher doses), priapism (males), testicular atrophy (males), virilization (females; including clitoromegaly, deepening of the voice in females)
Hematologic & oncologic: Clotting factors suppression, polycythemia, prostate carcinoma (males)
Hepatic: Abnormal hepatic function tests, cholestatic jaundice, hepatic insufficiency
Hypersensitivity: Anaphylactoid reaction (non-immunologic anaphylaxis), hypersensitivity reaction
<1%, postmarketing, and/or case reports: Hepatic coma, hepatocellular neoplasm, hepatotoxicity (idiosyncratic; Chalasani 2014), peliosis hepatitis
Warnings/Precautions
Concerns related to adverse effects:
- Dyslipidemia: Anabolic steroids may alter serum lipid profile; use caution in patients with history of myocardial infarction or coronary artery disease.
- Gynecomastia: May cause gynecomastia.
- Hepatic effects: Prolonged use of high doses of oral androgens has been associated with serious hepatic effects (eg, peliosis hepatis, hepatic neoplasms, cholestatic hepatitis, jaundice). Discontinue use in patients with cholestatic hepatitis with jaundice or abnormal liver function tests.
Disease-related concerns:
- Carbohydrate intolerance: May have adverse effects on glucose tolerance; use caution in patients with diabetes.
- Edematous conditions: Use with caution in patients with conditions influenced by edema (eg, cardiovascular disease, migraine, seizure disorder, renal impairment); may cause fluid retention.
- Heart failure: Not recommended for androgen replacement in hypogonadal males with uncontrolled or poorly controlled heart failure (Bhasin 2010).
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Hypercalcemia: Use with caution in patients with breast cancer or immobilization; may cause hypercalcemia by stimulating osteolysis. Discontinue use if hypercalcemia occurs; may indicate bony metastasis.
- Renal impairment: Use with caution in renal impairment; not recommended for androgen replacement in hypogonadal males with severe lower urinary tract symptoms (eg, International Prostate Symptom Score [IPSS] >19) (Bhasin 2010).
- Sleep apnea: Not recommended for androgen replacement in hypogonadal males with untreated severe obstructive sleep apnea (Bhasin 2010).
Special populations:
- Elderly: Elderly males may be at greater risk for prostatic hyperplasia and prostate cancer; use with caution.
- Pediatric: May accelerate bone maturation without producing compensatory gain in linear growth in children. In prepubertal children, perform radiographic examination of the hand and wrist every 6 months to determine the rate of bone maturation and to assess the effect of treatment on the epiphyseal centers.
- Women: During treatment for metastatic breast cancer, women should be monitored for signs of virilization (eg, deepening of voice, hirsutism, acne, clitoromegaly, menstrual irregularities); discontinue use with evidence of mild virilization to prevent irreversible symptoms.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Fertility: Large doses of exogenous androgens may suppress spermatogenesis; not recommended for androgen replacement in hypogonadal males desiring fertility (Bhasin 2010).
Monitoring Parameters
Periodic liver function tests, lipid panel, and serum glucose (diabetic patients); hemoglobin and hematocrit at baseline then periodically during therapy (alternatively in males receiving androgen replacement therapy, it has been recommended to monitor at baseline, at 3 to 6 months, and then annually [Bhasin 2010])
Urine and serum calcium and signs of virilization in females treated for breast cancer
Radiologic examination of wrist and hand every 6 months (prepubertal males); response to treatment and adverse events 3 to 6 months after initiation and then annually (males)
Signs/symptoms of edema, sleep apnea, and/or heart failure
Pregnancy
Pregnancy Risk Factor
X
Pregnancy Considerations
Use is contraindicated in women who are or may become pregnant. May cause androgenic effects to the female fetus; clitoral hypertrophy, labial fusion, urogenital sinus defect, vaginal atresia, and ambiguous genitalia have been reported.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience enlarged breasts (males), acne, decreased sex drive, anxiety, or headache. Have patient report immediately to prescriber signs of high calcium (weakness, confusion, feeling tired, headache, nausea and vomiting, constipation, or bone pain), signs of liver problems (dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes), signs of virilization (in females a deep voice, facial hair, pimples, or period changes), shortness of breath, excessive weight gain, swelling of arms or legs, skin discoloration, depression, burning or numbness feeling, nausea, vomiting, or erection that lasts more than 4 hours (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.