Boxed Warning
Hepatic injury:
There have been postmarketing reports of hospitalization and rarely death due to liver failure in patients taking flutamide. Evidence of hepatic injury included elevated serum transaminase levels, jaundice, hepatic encephalopathy and death related to acute hepatic failure. The hepatic injury was reversible after discontinuation of therapy in some patients. Approximately half of the reported cases occurred within the initial 3 months of treatment with flutamide.
Serum transaminase levels should be measured prior to starting treatment with flutamide. Flutamide is not recommended in patients whose ALT values exceed twice the upper limit of normal. Serum transaminase levels should then be measured monthly for the first 4 months of therapy, and periodically thereafter. Liver function tests also should be obtained at the first signs and symptoms suggestive of liver dysfunction (eg, nausea, vomiting, abdominal pain, fatigue, anorexia, “flu-like” symptoms, hyperbilirubinuria, jaundice, right upper quadrant tenderness). If at any time, a patient has jaundice, or their ALT rises above 2 times the upper limit of normal, flutamide should be immediately discontinued with close follow-up of liver function tests until resolution.
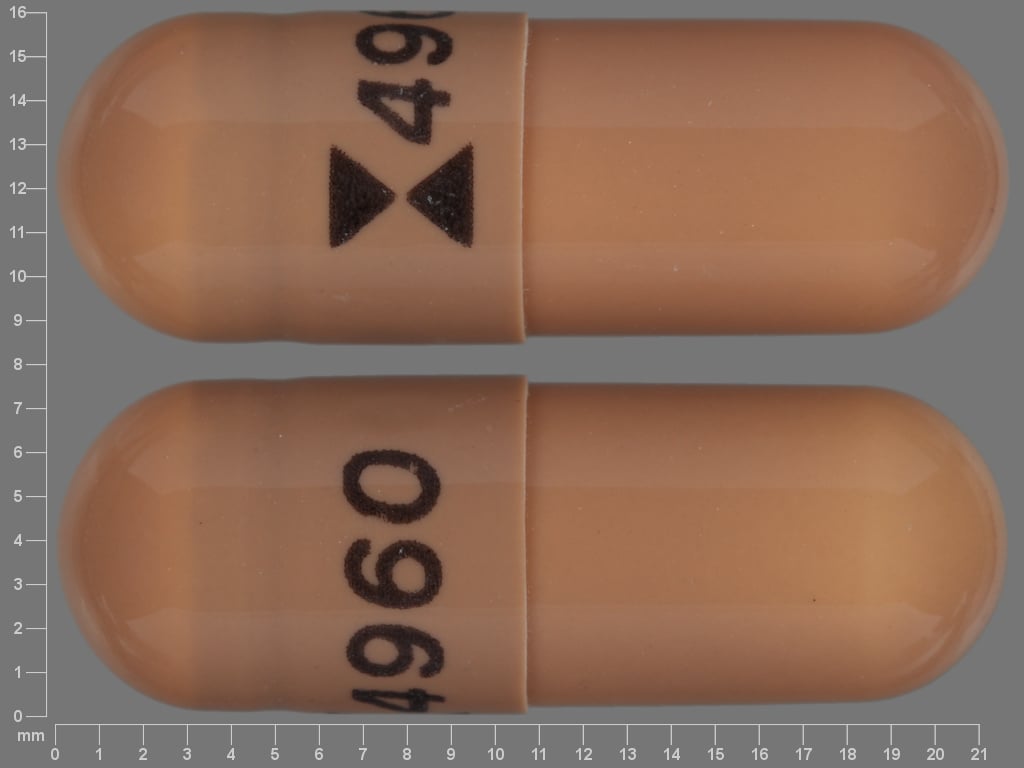
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Generic: 125 mg
Pharmacology
Mechanism of Action
Flutamide is a nonsteroidal antiandrogen that inhibits androgen uptake and/or inhibits binding of androgen in target tissues.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid and complete
Metabolism
Extensively hepatic to ≥6 metabolites, primarily 2-hydroxyflutamide (active)
Excretion
Primarily urine (as flutamide and metabolites); feces (~4%)
Time to Peak
~2 hours (2-hydroxyflutamide [active metabolite])
Half-Life Elimination
~6 hours (2-hydroxyflutamide [active metabolite])
Protein Binding
Parent drug: 94% to 96%; 2-hydroxyflutamide: 92% to 94%
Use in Specific Populations
Special Populations: Renal Function Impairment
The half-life of the active metabolite is slightly prolonged in patients with CrCl <29 mL/minute.
Special Populations: Elderly
The half-life is prolonged to ~9.6 hours (active metabolite at steady state).
Use: Labeled Indications
Prostate cancer (metastatic): Management of locally confined Stage B2 to C and Stage D2 metastatic prostate cancer (in combination with a luteinizing hormone-releasing hormone [LHRH] agonist). For Stage B2 to C prostate cancer, flutamide treatment (and goserelin) should start 8 weeks prior to initiating radiation therapy and continue during radiation therapy. To achieve treatment benefit in Stage D2 metastatic prostate cancer, initiate flutamide with the LHRH agonist and continue until disease progression.
Guideline recommendations: The American Society of Clinical Oncology and Cancer Care Ontario clinical practice guideline for systemic therapy in men with metastatic castration-resistant prostate cancer suggests that data regarding the clinical benefit of older antiandrogens (including flutamide) are limited, and that older antiandrogen agents may be less efficacious compared to contemporary antiandrogen agents. However, older antiandrogen agents may be offered in patients with low prostate cancer disease burden or limited therapy options (ASCO [Basch 2014]).
Contraindications
Hypersensitivity to flutamide or any component of the formulation; severe hepatic impairment (evaluate baseline hepatic enzymes prior to treatment).
Dosage and Administration
Dosing: Adult
Prostate cancer, metastatic (alternate agent; in patients with low disease burden): Oral: 250 mg 3 times daily (every 8 hours) in combination with a luteinizing hormone-releasing hormone agonist.
Dosing: Geriatric
Refer to adult dosing.
Administration
May be administered with or without food. Administer orally in 3 divided doses (every 8 hours).
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Dispense with a child-resistant closure in a tight, light-resistant container.
Flutamide Images
Drug Interactions
Choline C 11: Antiandrogens may diminish the therapeutic effect of Choline C 11. Monitor therapy
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Indium 111 Capromab Pendetide: Antiandrogens may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Adverse Reactions
>10%:
Endocrine & metabolic: Hot flash (46% to 61%), galactorrhea (9% to 42%), decreased libido (36%), increased lactate dehydrogenase (transient; mild)
Gastrointestinal: Diarrhea (12% to 40%), vomiting (11% to 12%)
Genitourinary: Impotence (33%), cystitis (16%), breast tenderness
Hematologic & oncologic: Rectal hemorrhage (14%), tumor flare
Hepatic: Increased serum AST (transient; mild)
1% to 10%:
Cardiovascular: Edema (4%), hypertension (1%)
Central nervous system: Anxiety, confusion, depression, dizziness, drowsiness, headache, insomnia, nervousness
Dermatologic: Skin rash (3% to 8%), ecchymoses, pruritus
Endocrine & metabolic: Gynecomastia (9%)
Gastrointestinal: Nausea (9%), proctitis (8%), gastric distress (4% to 6%), anorexia (4%), constipation, dyspepsia, increased appetite
Genitourinary: Hematuria (7%)
Hematologic & oncologic: Anemia (6%), leukopenia (3%), thrombocytopenia (1%)
Infection: Herpes zoster
Neuromuscular & skeletal: Weakness (1%)
<1%, postmarketing, and case reports: Cholestatic jaundice, hemolytic anemia, hepatic encephalopathy, hepatic failure, hepatic necrosis, hepatitis, hypersensitivity pneumonitis, increased blood urea nitrogen, increased gamma-glutamyl transferase, increased serum ALT, increased serum bilirubin, increased serum creatinine, jaundice, macrocytic anemia, malignant neoplasm of breast (male), methemoglobinemia, myocardial infarction, oligospermia, pulmonary embolism, skin photosensitivity, sulfhemoglobinemia, thrombophlebitis, urine discoloration (amber, yellow-green)
Warnings/Precautions
Concerns related to adverse effects:
- Aniline toxicity: 4-nitro-3-fluoro-methylaniline is a flutamide metabolite. Patients with G6PD deficiency, hemoglobin M disease, and/or smokers are at risk of toxicities associated with aniline exposure, including methemoglobinemia, hemolytic anemia, and cholestatic jaundice; consider monitoring methemoglobin levels.
- Gynecomastia: Gynecomastia may occur in patients receiving flutamide in combination with medical castration.
- Hepatic failure: [US Boxed Warning]: Postmarketing reports of hospitalization and death (rare) due to liver failure have been reported with flutamide. Evidence of hepatic injury included elevated serum transaminases, jaundice, hepatic encephalopathy, and death related to acute hepatic failure. Hepatotoxicity was reversible after discontinuation in some cases. In about half of reported cases, the onset of hepatotoxicity occurred within the first 3 months of flutamide treatment. Monitor serum transaminase levels at baseline, monthly for 4 months, and periodically thereafter. Obtain LFTs at the first symptoms suggestive of liver dysfunction (nausea, vomiting, abdominal pain, fatigue, anorexia, "flu-like" symptoms, hyperbilirubinuria, jaundice, or right upper quadrant tenderness). Use is not recommended in patients with ALT values >2 times ULN. Discontinue flutamide immediately in patients with jaundice or if ALT rises above 2 times ULN; closely monitor LFTs until resolution. Use is contraindicated in patients with severe hepatic impairment.
Disease-related concerns:
- Cardiovascular disease: Androgen-deprivation therapy may increase the risk for cardiovascular disease (Levine 2010).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Females: Flutamide is not indicated for use in females and should not be used in females, particularly for nonserious or non-life-threatening conditions.
Monitoring Parameters
Serum transaminases (at baseline, monthly for 4 months, and periodically thereafter); monitor liver function tests at the first sign or symptom of liver dysfunction (eg, nausea, vomiting, abdominal pain, fatigue, anorexia, flu-like symptoms, hyperbilirubinuria, jaundice, or right upper quadrant tenderness); monitor prostate specific antigen (PSA). Consider monitoring methemoglobin levels in patients with hemoglobin M disease or with G6PD deficiency and in smokers. Monitor adherence.
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
Based on the mechanism of action and data from animal reproduction studies, in utero exposure to flutamide may cause fetal harm.
Although flutamide is not indicated for use in females, it has been used off label for acne, hirsutism, polycystic ovary syndrome (PCOS), and female pattern hair loss in women. Due to the potential for serious toxicity and the availability of other treatment options, off-label use for these conditions is not recommended (Azarchi 2019; ES [Goodman 2015]); ES [Martin 2018]). Effective contraception is recommended if used in females for these conditions (Azarchi 2019).
Women treated with flutamide for PCOS may have a return of regular menses and ovulatory cycles (Paradisi 2013).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience hot flashes, nausea, vomiting, enlarged breasts, decreased sex drive, or sexual dysfunction. Have patient report immediately to prescriber signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), blood in the urine, shortness of breath, blue/gray skin discoloration, rectal pain, rectal bleeding, severe loss of strength and energy, or severe diarrhea (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.