If you and your partner are struggling to have a baby, you're not alone. In the United States, 10% to 15% of couples are infertile. Infertility is defined as not being able to get pregnant despite having frequent, unprotected sex for at least a year for most couples.
Infertility may result from an issue with either you or your partner, or a combination of factors that prevent pregnancy. Fortunately, there are many safe and effective therapies that significantly improve your chances of getting pregnant.
Symptoms
The main symptom of infertility is not getting pregnant. There may be no other obvious symptoms. Sometimes, women with infertility may have irregular or absent menstrual periods. In some cases, men with infertility may have some signs of hormonal problems, such as changes in hair growth or sexual function.
Most couples will eventually conceive, with or without treatment.
When to see a doctor
You probably don't need to see your health care provider about infertility unless you have been trying regularly to get pregnant for at least one year. Women should talk with a care provider earlier, however, if they:
- Are age 35 or older and have been trying to conceive for six months or longer
- Are over age 40
- Have irregular or absent periods
- Have very painful periods
- Have known fertility problems
- Have been diagnosed with endometriosis or pelvic inflammatory disease
- Have had multiple miscarriages
- Have undergone treatment for cancer
Men should talk to a health care provider if they have:
- A low sperm count or other problems with sperm
- A history of testicular, prostate or sexual problems
- Undergone treatment for cancer
- Small testicles or swelling in the scrotum
- Others in your family with infertility problems
Causes
All of the steps during ovulation and fertilization need to happen correctly in order to get pregnant. Sometimes the issues that cause infertility in couples are present at birth, and sometimes they develop later in life.
Infertility causes can affect one or both partners. Sometimes, no cause can be found.
Causes of male infertility
These may include:
- Abnormal sperm production or function due to undescended testicles, genetic defects, health problems such as diabetes, or infections such as chlamydia, gonorrhea, mumps or HIV. Enlarged veins in the testes (varicocele) also can affect the quality of sperm.
- Problems with the delivery of sperm due to sexual problems, such as premature ejaculation; certain genetic diseases, such as cystic fibrosis; structural problems, such as a blockage in the testicle; or damage or injury to the reproductive organs.
- Overexposure to certain environmental factors, such as pesticides and other chemicals, and radiation. Cigarette smoking, alcohol, marijuana, anabolic steroids, and taking medications to treat bacterial infections, high blood pressure and depression also can affect fertility. Frequent exposure to heat, such as in saunas or hot tubs, can raise body temperature and may affect sperm production.
- Damage related to cancer and its treatment, including radiation or chemotherapy. Treatment for cancer can impair sperm production, sometimes severely.
Causes of female infertility
Causes of female infertility may include:
- Ovulation disorders, which affect the release of eggs from the ovaries. These include hormonal disorders such as polycystic ovary syndrome. Hyperprolactinemia, a condition in which you have too much prolactin — the hormone that stimulates breast milk production — also may interfere with ovulation. Either too much thyroid hormone (hyperthyroidism) or too little (hypothyroidism) can affect the menstrual cycle or cause infertility. Other underlying causes may include too much exercise, eating disorders or tumors.
- Uterine or cervical abnormalities, including abnormalities with the cervix, polyps in the uterus or the shape of the uterus. Noncancerous (benign) tumors in the uterine wall (uterine fibroids) may cause infertility by blocking the fallopian tubes or stopping a fertilized egg from implanting in the uterus.
- Fallopian tube damage or blockage, often caused by inflammation of the fallopian tube (salpingitis). This can result from pelvic inflammatory disease, which is usually caused by a sexually transmitted infection, endometriosis or adhesions.
- Endometriosis, which occurs when endometrial tissue grows outside of the uterus, may affect the function of the ovaries, uterus and fallopian tubes.
- Primary ovarian insufficiency (early menopause), when the ovaries stop working and menstruation ends before age 40. Although the cause is often unknown, certain factors are associated with early menopause, including immune system diseases, certain genetic conditions such as Turner syndrome or carriers of Fragile X syndrome, and radiation or chemotherapy treatment.
- Pelvic adhesions, bands of scar tissue that bind organs that can form after pelvic infection, appendicitis, endometriosis or abdominal or pelvic surgery.
- Cancer and its treatment. Certain cancers — particularly reproductive cancers — often impair female fertility. Both radiation and chemotherapy may affect fertility.
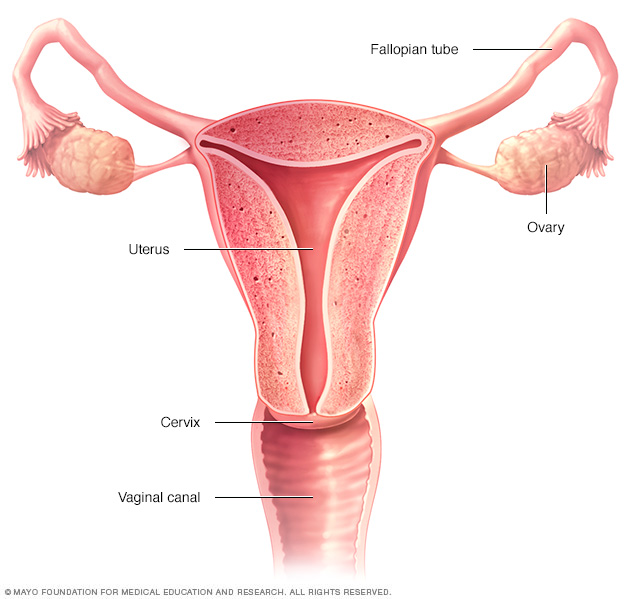
The ovaries, fallopian tubes, uterus, cervix and vagina (vaginal canal) make up the female reproductive system.
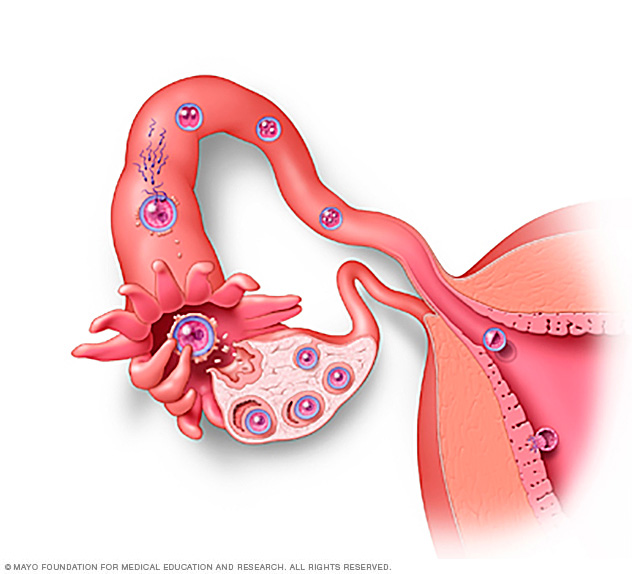
During fertilization, the sperm and egg unite in one of the fallopian tubes to form a zygote. Then the zygote travels down the fallopian tube, where it becomes a morula. Once it reaches the uterus, the morula becomes a blastocyst. The blastocyst then burrows into the uterine lining — a process called implantation.
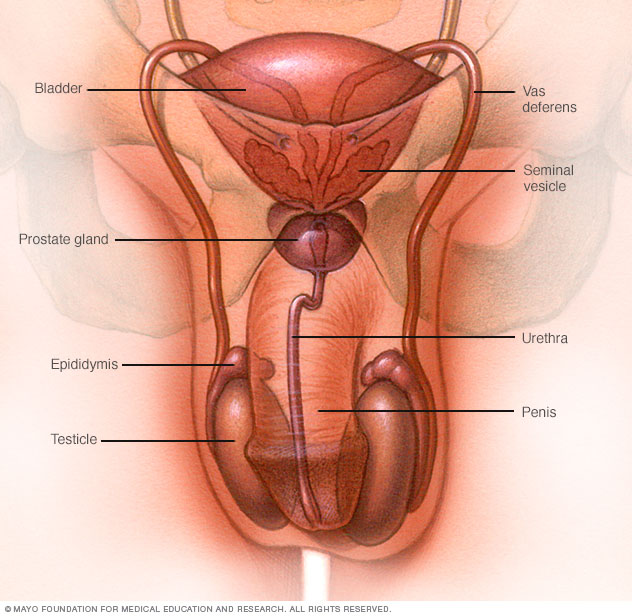
The male reproductive system makes, stores and moves sperm. Testicles produce sperm. Fluid from the seminal vesicles and prostate gland combine with sperm to make semen. The penis ejaculates semen during sexual intercourse.
Risk factors
Many of the risk factors for both male and female infertility are the same. They include:
- Age. Women's fertility gradually declines with age, especially in the mid-30s, and it drops rapidly after age 37. Infertility in older women is likely due to the lower number and quality of eggs, and can also be due to health problems that affect fertility. Men over age 40 may be less fertile than younger men.
- Tobacco use. Smoking tobacco or marijuana by either partner may reduce the likelihood of pregnancy. Smoking also reduces the possible effectiveness of fertility treatment. Miscarriages are more frequent in women who smoke. Smoking can increase the risk of erectile dysfunction and a low sperm count in men.
- Alcohol use. For women, there's no safe level of alcohol use during conception or pregnancy. Alcohol use may contribute to infertility. For men, heavy alcohol use can decrease sperm count and motility.
- Being overweight. Among American women, an inactive lifestyle and being overweight may increase the risk of infertility. For men, sperm count also may be affected by being overweight.
- Being underweight. Women at risk of fertility problems include those with eating disorders, such as anorexia or bulimia, and those who follow a very low-calorie or restrictive diet.
- Exercise issues. A lack of exercise contributes to obesity, which increases the risk of infertility. Less often, ovulation problems may be associated with frequent strenuous, intense exercise in women who are not overweight.
Prevention
Some types of infertility aren't preventable. But several strategies may increase your chances of pregnancy.
Couples
Have regular intercourse several times around the time of ovulation for the highest pregnancy rate. Intercourse beginning at least five days before and until a day after ovulation improves your chances of getting pregnant. Ovulation usually occurs in the middle of the cycle — halfway between menstrual periods — for most women with menstrual cycles about 28 days apart.
Men
Although most types of infertility aren't preventable in men, these strategies may help:
- Avoid drug and tobacco use and drinking too much alcohol, which may contribute to male infertility.
- Avoid high temperatures found in hot tubs and hot baths, as they can temporarily affect sperm production and motility.
- Avoid exposure to industrial or environmental toxins, which can affect sperm production.
- Limit medications that may impact fertility, both prescription and nonprescription drugs. Talk with your doctor about any medications you take regularly, but don't stop taking prescription medications without medical advice.
- Exercise moderately. Regular exercise may improve sperm quality and increase the chances for achieving a pregnancy.
Women
For women, a number of strategies may increase the chances of becoming pregnant:
- Quit smoking. Tobacco has many negative effects on fertility, not to mention your general health and the health of a fetus. If you smoke and are considering pregnancy, quit now.
- Avoid alcohol and street drugs. These substances may impair your ability to conceive and have a healthy pregnancy. Don't drink alcohol or use recreational drugs, such as marijuana, if you're trying to get pregnant.
- Limit caffeine. Women trying to get pregnant may want to limit caffeine intake. Ask your doctor for guidance on the safe use of caffeine.
- Exercise moderately. Regular exercise is important, but exercising so intensely that your periods are infrequent or absent can affect fertility.
- Avoid weight extremes. Being overweight or underweight can affect your hormone production and cause infertility.
Diagnosis
Before infertility testing, your doctor or clinic works to understand your sexual habits and may make recommendations to improve your chances of getting pregnant. In some infertile couples, no specific cause is found (unexplained infertility).
Infertility evaluation can be expensive, and sometimes involves uncomfortable procedures. Some medical plans may not cover the cost of fertility treatment. Finally, there's no guarantee — even after all the testing and counseling — that you'll get pregnant.
Tests for men
Male fertility requires that the testicles produce enough healthy sperm, and that the sperm is ejaculated effectively into the vagina and travels to the egg. Tests for male infertility attempt to determine whether any of these processes are impaired.
You may have a general physical exam, including examination of your genitals. Specific fertility tests may include:
- Semen analysis. Your doctor may ask for one or more semen specimens. Semen is generally obtained by masturbating or by interrupting intercourse and ejaculating your semen into a clean container. A lab analyzes your semen specimen. In some cases, urine may be tested for the presence of sperm.
- Hormone testing. You may have a blood test to determine your level of testosterone and other male hormones.
- Genetic testing. Genetic testing may be done to determine whether there's a genetic defect causing infertility.
- Testicular biopsy. In select cases, a testicular biopsy may be performed to identify abnormalities contributing to infertility or to retrieve sperm for assisted reproductive techniques, such as IVF.
- Imaging. In certain situations, imaging studies such as a brain MRI, transrectal or scrotal ultrasound, or a test of the vas deferens (vasography) may be performed.
- Other specialty testing. In rare cases, other tests to evaluate the quality of the sperm may be performed, such as evaluating a semen specimen for DNA abnormalities.
Tests for women
Fertility for women relies on the ovaries releasing healthy eggs. The reproductive tract must allow an egg to pass into the fallopian tubes and join with sperm for fertilization. The fertilized egg must travel to the uterus and implant in the lining. Tests for female infertility try to find out if any of these processes are impaired.
You may have a general physical exam, including a regular gynecological exam. Specific fertility tests may include:
- Ovulation testing. A blood test measures hormone levels to determine whether you're ovulating.
- Hysterosalpingography. Hysterosalpingography (his-tur-o-sal-ping-GOG-ruh-fee) evaluates the condition of your uterus and fallopian tubes and looks for blockages or other problems. X-ray contrast is injected into your uterus, and an X-ray is taken to determine if the cavity is normal and to see if the fluid spills out of your fallopian tubes.
- Ovarian reserve testing. This testing helps determine the quantity of the eggs available for ovulation. This approach often begins with hormone testing early in the menstrual cycle.
- Other hormone testing. Other hormone tests check levels of ovulatory hormones, as well as pituitary hormones that control reproductive processes.
- Imaging tests. Pelvic ultrasound looks for uterine or ovarian disease. Sometimes a sonohysterogram, also called a saline infusion sonogram, is used to see details inside the uterus that are not seen on a regular ultrasound.
Depending on your situation, rarely your testing may include:
- Hysteroscopy. Depending on your symptoms, your doctor may request a hysteroscopy to look for uterine disease. During the procedure, your doctor inserts a thin, lighted device through your cervix into your uterus to view any potential abnormalities.
- Laparoscopy. This minimally invasive surgery involves making a small incision beneath your navel and inserting a thin viewing device to examine your fallopian tubes, ovaries and uterus. A laparoscopy may identify endometriosis, scarring, blockages or irregularities of the fallopian tubes, and problems with the ovaries and uterus.
Not everyone needs to have all, or even many, of these tests before the cause of infertility is found. You and your doctor will decide which tests you will have and when.
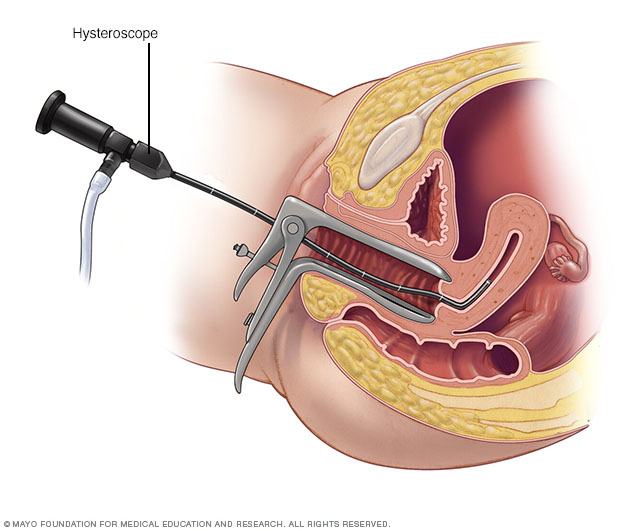
During a hysteroscopy, your provider uses a thin, lighted instrument (hysteroscope) to view the inside of your uterus.
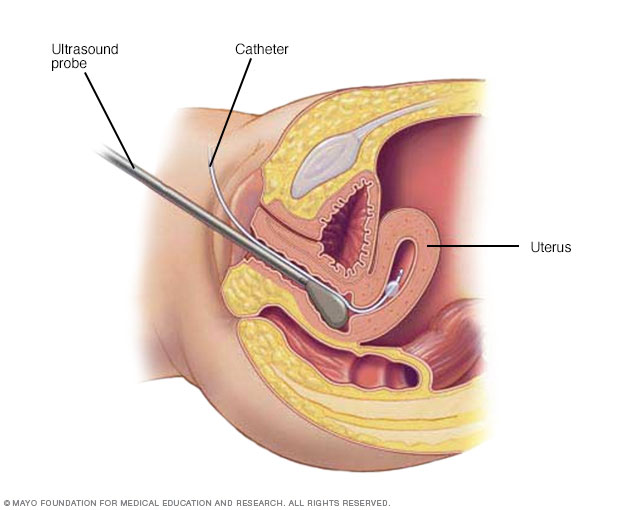
During hysterosonography (his-tur-o-suh-NOG-ruh-fee), your doctor uses a thin, flexible tube (catheter) to inject salt water (saline) into the hollow part of your uterus. Using an ultrasound probe, your doctor obtains images of the inside of your uterus and checks for any irregularities.
Treatment
Infertility treatment depends on:
- What's causing the infertility
- How long you've been infertile
- Your age and your partner's age
- Personal preferences
Some causes of infertility can't be corrected.
In cases where spontaneous pregnancy doesn't happen, couples can often still achieve a pregnancy through use of assisted reproductive technology. Infertility treatment may involve significant financial, physical, psychological and time commitments.
Treatment for men
Men's treatment for general sexual problems or lack of healthy sperm may include:
- Changing lifestyle factors. Improving lifestyle and certain behaviors can improve chances for pregnancy, including discontinuing select medications, reducing or eliminating harmful substances, improving frequency and timing of intercourse, exercising regularly, and optimizing other factors that may otherwise impair fertility.
- Medications. Certain medications may improve sperm count and likelihood for achieving a successful pregnancy. These medicines may increase testicular function, including sperm production and quality.
- Surgery. For some conditions, surgery may be able to reverse a sperm blockage and restore fertility. In other cases, surgically repairing a varicocele may improve overall chances for pregnancy.
- Sperm retrieval. These techniques obtain sperm when ejaculation is a problem or when no sperm are present in the ejaculated fluid. They may also be used in cases in which assisted reproductive techniques are planned and sperm counts are low or otherwise abnormal.
Treatment for women
Some women need only one or two therapies to improve fertility. Other women may need several different types of treatment to achieve pregnancy.
- Stimulating ovulation with fertility drugs. Fertility drugs are the main treatment for women who are infertile due to ovulation disorders. These medications regulate or induce ovulation. Talk with your doctor about fertility drug options — including the benefits and risks of each type.
- Intrauterine insemination (IUI). During IUI, healthy sperm are placed directly in the uterus around the time the ovary releases one or more eggs to be fertilized. Depending on the reasons for infertility, the timing of IUI can be coordinated with your normal cycle or with fertility medications.
- Surgery to restore fertility. Uterine problems such as endometrial polyps, a uterine septum, intrauterine scar tissue and some fibroids can be treated with hysteroscopic surgery. Endometriosis, pelvic adhesions, and larger fibroids may require laparoscopic surgery or surgery with a larger incision of the abdomen.
Assisted reproductive technology
Assisted reproductive technology (ART) is any fertility treatment in which the egg and sperm are handled. There are several types of ART.
In vitro fertilization (IVF) is the most common ART technique. IVF involves stimulating and retrieving multiple mature eggs, fertilizing them with sperm in a dish in a lab, and implanting the embryos in the uterus several days after fertilization.
Other techniques are sometimes used in an IVF cycle, such as:
- Intracytoplasmic sperm injection (ICSI). A single healthy sperm is injected directly into a mature egg. ICSI is often used when there is poor semen quality or quantity, or if fertilization attempts during prior IVF cycles failed.
- Assisted hatching. This technique assists the implantation of the embryo into the lining of the uterus by opening the outer covering of the embryo (hatching).
- Donor eggs or sperm. Most ART is done using a couple's own eggs and sperm. However, if there are severe problems with either the eggs or the sperm, you may choose to use eggs, sperm or embryos from a known or anonymous donor.
- Gestational carrier. Women who don't have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using a gestational carrier. In this case, the couple's embryo is placed in the uterus of the carrier for pregnancy.
Complications of treatment
Complications of infertility treatment may include:
- Multiple pregnancy. The most common complication of infertility treatment is a multiple pregnancy — twins, triplets or more. Generally, the greater the number of fetuses, the higher the risk of premature labor and delivery, as well as problems during pregnancy such as gestational diabetes. Babies born prematurely are at increased risk of health and developmental problems. Talk to your doctor about any concerns you have about a multiple pregnancy before starting treatment.
- Ovarian hyperstimulation syndrome (OHSS). Fertility medications to induce ovulation can cause OHSS, particularly with ART, in which the ovaries become swollen and painful. Symptoms may include mild abdominal pain, bloating, and nausea that lasts about a week, or longer if you become pregnant. Rarely, a more severe form causes rapid weight gain and shortness of breath requiring emergency treatment.
- Bleeding or infection. As with any invasive procedure, there is a rare risk of bleeding or infection with assisted reproductive technology or reproductive surgery.

During in vitro fertilization, eggs are removed from mature follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg (embryo) is transferred into the uterus (C).
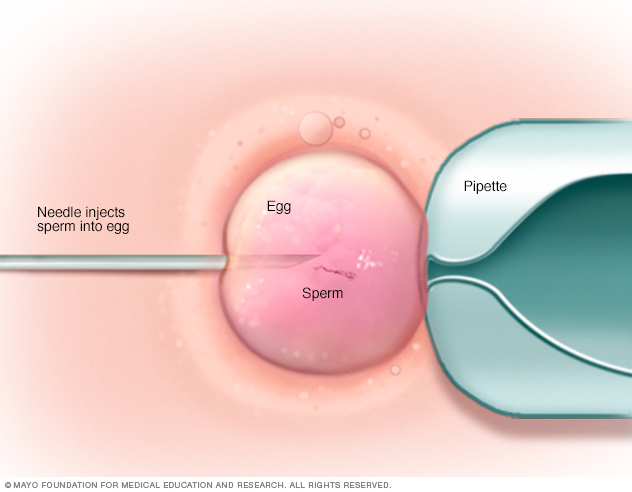
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg. ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
Coping and support
Coping with infertility can be extremely difficult because there are so many unknowns. The journey can take an emotional toll on a couple. Taking these steps can help you cope:
- Be prepared. The uncertainty of infertility testing and treatments can be difficult and stressful. Ask your doctor to explain the steps, and prepare for each one.
- Set limits. Decide before starting treatment which procedures, and how many, are emotionally and financially acceptable for you and your partner. Fertility treatments may be expensive and often are not covered by insurance companies, and a successful pregnancy often depends on repeated attempts.
- Consider other options. Determine alternatives — donor sperm or egg, gestational carrier or adoption, or even having no children — as early as possible in the infertility evaluation. This may reduce anxiety during treatments and feelings of hopelessness if conception doesn't occur.
- Seek support. Locate support groups or counseling services for help before and after treatment to help endure the process and ease the grief should treatment fail.
Managing emotional stress during treatment
Try these strategies to help manage emotional stress during treatment:
- Express yourself. Reaching out to others can help you deal with guilt or anger.
- Stay in touch with loved ones. Talking to your partner, family and friends can be very beneficial. The best support often comes from loved ones and those closest to you.
- Reduce stress. Some studies have shown that couples experiencing psychological stress had poorer results with infertility treatment. Try to reduce stress in your life before trying to become pregnant.
- Exercise and eat a healthy diet. Keeping up a moderate exercise routine and a healthy diet can improve your outlook and keep you focused on living your life.
Managing emotional effects of the outcome
You'll face the possibility of psychological challenges no matter your results:
- Not achieving pregnancy, or having a miscarriage. The emotional stress of not being able to have a baby can be devastating even in the most loving and affectionate relationships.
- Success. Even if fertility treatment is successful, it's common to experience stress and fear of failure during pregnancy. If you have a history of depression or anxiety disorder, you're at increased risk of these problems recurring in the months after your child's birth.
- Multiple births. A successful pregnancy that results in multiple births introduces medical complexities and the likelihood of significant emotional stress both during pregnancy and after delivery.
Seek professional help if the emotional impact of the outcome of your fertility treatments becomes too heavy for you or your partner.
Preparing for an appointment
Depending on your age and personal health history, your doctor may recommend a medical evaluation. A gynecologist, urologist or family doctor can help determine whether there's a problem that requires a specialist or clinic that treats infertility problems. In some cases, both you and your partner may require a comprehensive infertility evaluation.
What you can do
To get ready for your first appointment:
- Provide details about your attempts to get pregnant. Write down details about when you started trying to conceive and how often you've had intercourse, especially around the midpoint of your cycle — the time of ovulation.
- Bring your key medical information. Include any other medical conditions you or your partner has, as well as information about any previous infertility evaluations or treatments.
- Make a list of any medications, vitamins, herbs or other supplements you take. Include the doses and how often you take them.
- Make a list of questions to ask your doctor. List the most important questions first in case time runs short.
For infertility, some basic questions to ask your doctor include:
- What are the possible reasons we haven't yet conceived?
- What kinds of tests do we need?
- What treatment do you recommend trying first?
- What side effects are associated with the treatment you're recommending?
- What is the likelihood of conceiving multiple babies with the treatment you're recommending?
- For how many cycles will we try this treatment?
- If the first treatment doesn't work, what will you recommend trying next?
- Are there any long-term complications associated with this or other infertility treatments?
Don't hesitate to ask your doctor to repeat information or to ask follow-up questions.
What to expect from your doctor
Be ready to answer questions to help your doctor quickly determine next steps in making a diagnosis and starting care.
Questions for couples
Possible questions for couples include:
- How long have you been actively trying to get pregnant?
- How often do you have intercourse?
- Do you use any lubricants during sex?
- Do either of you smoke?
- Do either of you use alcohol or recreational drugs? How often?
- Are either of you currently taking any medications, dietary supplements or anabolic steroids?
- Have either of you been treated for any other medical conditions, including sexually transmitted infections?
Questions for men
Your doctors may ask:
- Do you have any difficulties putting on muscle or do you take any substances to increase muscle mass?
- Do you ever notice a fullness in the scrotum, particularly after standing for extended periods of time?
- Do you experience any testicular pain or pain after ejaculation?
- Have you had any sexual problems, such as difficulty maintaining an erection, ejaculating too soon, not being able to ejaculate or reduced sexual desire?
- Have you conceived a child with any previous partners?
- Do you regularly take hot baths or steam baths?
Questions for the woman
Your doctors may ask:
- At what age did you start menstruating?
- What are your cycles typically like? How regular, long and heavy are they?
- Have you ever been pregnant before?
- Have you been charting your cycles or testing for ovulation? If so, for how many cycles?
- What is your typical daily diet?
- Do you exercise regularly? How much?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.