Pulmonary valve stenosis is a narrowing of the valve located between the lower right heart chamber (right ventricle) and the lung arteries (pulmonary arteries). In a narrowed heart valve, the valve flaps (cusps) may become thick or stiff. This reduces blood flow through the valve.
Usually, pulmonary valve disease results from a heart problem that develops before birth (congenital heart defect). However, adults may develop pulmonary valve stenosis as a complication of another illness.
Pulmonary valve stenosis ranges from mild to severe. Some people with mild pulmonary valve stenosis don't notice any symptoms and may only require occasional doctor's checkups. Moderate and severe pulmonary valve stenosis may require a procedure to repair or replace the valve.
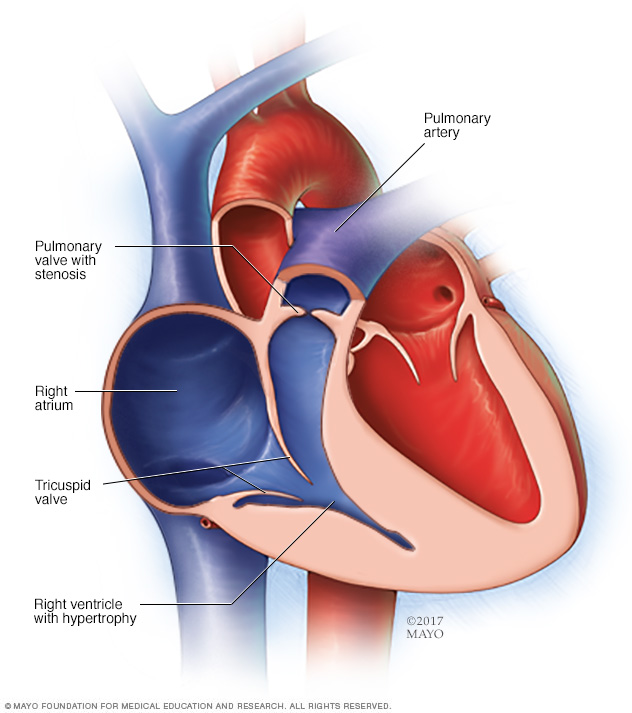
In pulmonary stenosis, narrowing of the pulmonary valve blocks blood flow from the lower right lower chamber (right ventricle) to the lung (pulmonary) arteries. The greater the narrowing, the harder the right ventricle must work to pump blood to the lungs. The increased pressure causes the right ventricle to become thick.
Symptoms
Pulmonary valve stenosis signs and symptoms vary, depending on how much blood flow is blocked. Some people with mild pulmonary stenosis don't have symptoms. Those with more-severe pulmonary stenosis may first notice symptoms while exercising.
Pulmonary valve stenosis signs and symptoms may include:
- A whooshing sound (murmur) that can be heard with a stethoscope
- Fatigue
- Shortness of breath, especially during activity
- Chest pain
- Loss of consciousness (fainting)
Babies with pulmonary valve stenosis and other congenital heart defects may appear blue (cyanotic).
When to see a doctor
Talk to your doctor if you or your child has:
- Shortness of breath
- Chest pain
- Fainting
If you or your child has pulmonary stenosis or another heart problem, prompt diagnosis and treatment can help reduce the risk of complications.
Causes
Pulmonary valve stenosis is most often a congenital heart defect. The exact cause is unclear. The pulmonary valve doesn't develop properly as the baby is growing in the womb.
The pulmonary valve is made of three thin pieces of tissue called flaps (cusps). The cusps open and close with each heartbeat and make sure blood moves in the right direction.
In pulmonary valve stenosis, one or more of the cusps may be stiff or thick, or the cusps may be joined (fused) together. As a result, the valve doesn't open fully. The smaller valve opening makes it harder for blood to flow out of the lower right heart chamber (right ventricle). Pressure increases inside the right ventricle as it tries to push blood through the smaller opening. The increased pressure creates a strain on the heart that eventually causes the right ventricle's muscular wall to thicken.
Risk factors
Conditions or disorders that may increase the risk of pulmonary valve stenosis include:
- German measles (rubella). Having German measles (rubella) during pregnancy increases the risk of pulmonary valve stenosis in the baby.
- Noonan syndrome. This genetic disorder causes various problems with the heart's structure and function.
- Rheumatic fever. This complication of strep throat can cause permanent damage to the heart, including the heart valves. It can increase the risk of developing pulmonary valve stenosis later in life.
- Carcinoid syndrome. A rare cancerous tumor releases certain chemicals into the bloodstream, causing shortness of breath, flushing and other signs and symptoms. Some people with this syndrome develop carcinoid heart disease, which damages heart valves.
Complications
Possible complications of pulmonary stenosis include:
- Infection of the lining of the heart (infective endocarditis). People with heart valve problems, such as pulmonary stenosis, have an increased risk of developing bacterial infections that affect the inner lining of the heart.
- Irregular heartbeat (arrhythmia). People with pulmonary stenosis are more likely to have an irregular heartbeat. Unless the stenosis is severe, irregular heartbeats due to pulmonary stenosis usually aren't life-threatening.
- Thickening of the heart muscle. In severe pulmonary stenosis, the heart's right ventricle must pump harder to force blood into the pulmonary artery. The strain on the heart causes the muscular wall of the ventricle to thicken (right ventricular hypertrophy).
- Heart failure. If the right ventricle can't pump properly, heart failure eventually develops. Symptoms of heart failure include fatigue, shortness of breath, and swelling of the legs and abdomen.
- Pregnancy complications. The risks of complications during labor and delivery are higher for those with severe pulmonary valve stenosis than those without the condition.
Diagnosis
Pulmonary valve stenosis is often diagnosed in childhood. However, it may not be detected until later in life.
The doctor will use a stethoscope to listen to your or your child's heart. A whooshing sound (murmur) caused by choppy (turbulent) blood flow across the narrowed valve may be heard.
Tests to diagnose pulmonary valve stenosis may include:
- Electrocardiogram (ECG or EKG). This quick and painless test records the electrical signals in the heart. Sticky patches (electrodes) are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which displays the test results. An ECG can show how the heart is beating and may reveal signs of heart muscle thickening.
- Echocardiogram. An echocardiogram uses sound waves to produce images of the heart. This common test allows a doctor to see how the heart beats and pumps blood. An echocardiogram can show the structure of the pulmonary valve and the location and severity of any valve narrowing.
-
Cardiac catheterization. A thin tube (catheter) is inserted into the groin and threaded through the blood vessels to the heart. Dye can be injected through the catheter into the blood vessels to make them more visible on X-rays (coronary angiogram).
Doctors also use cardiac catheterization to measure pressure within the chambers of the heart to see how forcefully blood pumps through the heart. If you've been diagnosed with pulmonary valve stenosis, your doctor can determine how severe the condition is by comparing the difference in blood pressure between the right lower heart chamber and the pulmonary artery.
- Other imaging tests. Magnetic resonance imaging (MRI) and computed tomography (CT) scans are sometimes used to confirm the diagnosis of pulmonary valve stenosis.
Treatment
If you have mild pulmonary valve stenosis without symptoms, you may only need occasional doctor's checkups.
If you have moderate or severe pulmonary valve stenosis, you may need a heart procedure or heart surgery. The type of procedure or surgery you have depends on your overall health and the appearance of your pulmonary valve.
Heart procedures and surgery used to treat pulmonary valve stenosis include:
-
Balloon valvuloplasty. The doctor inserts a flexible tube (catheter) with a balloon on the tip into an artery, usually in the groin. X-rays are used to help guide the catheter to the narrowed valve in the heart. The doctor inflates the balloon, which widens the valve opening, and separates the valve flaps, if needed. The balloon is then deflated. The catheter and balloon are removed.
Valvuloplasty may improve blood flow through the heart and reduce pulmonary valve stenosis symptoms. However, the valve may narrow again. Some people need valve repair or replacement in the future.
-
Pulmonary valve replacement. If balloon valvuloplasty isn't an option, open-heart surgery or a catheter procedure may be done to replace the pulmonary valve. If there are other congenital heart defects, the doctor can often repair those during the same surgery.
People who have had pulmonary valve replacement need to take antibiotics before certain dental procedures or surgeries to prevent endocarditis.
Lifestyle and home remedies
If you have valve disease, it's important to take steps to keep your heart healthy. Certain lifestyle changes can decrease your risk of developing other types of heart disease or having a heart attack.
Lifestyle changes to talk to your doctor about include:
- Quitting smoking
- Eating a heart-healthy diet that includes fruits and vegetables, low-fat dairy products, whole grains, and lean meat
- Maintaining a healthy weight
- Getting regular exercise
Preparing for an appointment
If you or your child has valve disease, you will be referred to a doctor trained in evaluating and treating heart conditions (cardiologist).
Here's some information to help you get ready for your appointment.
What you can do
- Write down symptoms you or your child has, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including major stresses or recent illnesses.
- List all medications, vitamins and supplements you or your child takes.
- Write down questions to ask the doctor.
Preparing a list of questions can help you make the most of your time with your doctor. For pulmonary valve stenosis, some basic questions include:
- What's the most likely cause of my or my child's symptoms?
- Are there other possible causes?
- What tests are needed? Do these tests require any special preparation?
- Is pulmonary valve stenosis temporary or long lasting?
- What treatments are available, and which do you recommend?
- What are the risks of a balloon valvuloplasty or open-heart surgery?
- Do I need to restrict my or my child's activity?
- Are there brochures or other printed material that I can take? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, including:
- When did symptoms begin?
- Do the symptoms come and go, or are they continuous?
- Do the symptoms get worse during activity or when lying down?
- Does anything seem to improve symptoms?
Copyright © 1998-2025 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.